- Faculty Logins
- Student Portal
- COVID-19 Info
We’re enrolling for all classes! Email [email protected] for more information.
Indigenous Peoples Land Acknowledgement
Visit us on our social media pages! Facebook , Instagram , and Twitter
AIAM is switching from clinic booking in MindBody to booking in MangoMint! Watch for an email!
- About Our Programs
- Acupuncture
- Medical Massage Therapy
- Registered Nursing
- Practical Nursing
- 24 Months RN Program
- Admission Requirements
- Returning Alumni
- About Financial Aid

Holistic Needs Assessment: Everything You Need To Know
31 Jan, 2023 | By: Diane Sater-Wee
Imagine a world where every individual’s unique needs are understood and met comprehensively and holistically, where no one falls through the cracks, and everyone can thrive. That is the vision of a holistic needs assessment, a powerful tool that goes beyond surface-level evaluations to truly understand and address the complexities of an individual’s life. Holistic assessment in nursing is a comprehensive and holistic approach to evaluating a patient’s overall health and well-being.
What Is a Holistic Needs Assessment?
Simply put, a holistic needs assessment is the evaluation of an individual’s general well-being. It tackles various aspects that may impact a person’s health, such as the physical, mental, social, financial, and living environment. This approach aims to identify any areas of concern and develop a comprehensive plan of care that addresses all of the individual’s needs.
Adopting a holistic approach in healthcare can have several benefits for both the patient and the healthcare provider. Some of the key benefits include:
- Improved patient outcomes
- Increased patient satisfaction
- Improved communication and collaboration
What Is Included in a Holistic Needs Assessment?

The holistic needs assessment is an in-depth evaluation that considers all aspects of an individual’s well-being and identifies potential barriers to achieving optimal health. A holistic needs assessment typically includes the following elements:
Physical health: Examines an individual’s overall physical condition, including any medical conditions, medications being taken, and any physical limitations that may affect their daily activities.
Mental health: Evaluates the patient’s emotional, psychological, and cognitive well-being, including any mental health conditions or disorders.
Social and environmental factors: Assessment of an individual’s social support network, living conditions, and access to resources and services.
The caregiver’s needs: Includes an assessment of the needs of family members and caregivers who are providing support and assistance to the patient.
Risk factors: Assessment of any risk factors that may impact the individual’s well-being, such as poverty, isolation, or lack of access to healthcare.
Who Should Do a Holistic Needs Assessment?
Anyone who wants to have a comprehensive understanding of their overall well-being or would like to identify areas for improvement can greatly benefit from a holistic needs assessment.
A holistic needs assessment can help individuals who wish to improve their sense of purpose and fulfillment, especially those dealing with chronic health conditions, experiencing stress or emotional challenges, or seeking to improve their physical, emotional, and spiritual well-being. It can also aid those interested in making lifestyle changes, such as starting a new exercise or nutrition program.
What Happens at a Holistic Needs Assessment?

A holistic needs assessment is a comprehensive evaluation of a person’s physical, mental, emotional, and social well-being. It is performed by a team of healthcare professionals, such as doctors, nurses, social workers, and mental health professionals.
During a holistic needs assessment, the healthcare team will gather information about the person’s medical history, current symptoms, and overall functioning. They may also conduct physical exams, psychological assessments, and other diagnostic tests.
The healthcare team will also evaluate the person’s social and emotional needs, including their living situation, support system, and access to resources. They may also assess the person’s level of autonomy and ability to make decisions for themselves.
Based on the information gathered during the assessment, the healthcare team will develop a plan of care that addresses the patient’s physical, mental, emotional, and social needs. This plan may include medical treatment, therapy, rehabilitation, and other interventions.
Throughout the process, the healthcare team works closely with the patient and their family or caretaker. This collaboration helps ensure that the patient’s needs are met and that they are actively involved in the decision-making process.
How Long Does a Holistic Needs Assessment Take?
The time required for a holistic needs assessment varies depending on the complexity of the individual’s needs, the number of professionals involved in the assessment process, and the methods used to gather and analyze information. On average, it may take several weeks to complete.
The process includes planning and organizing the assessment, conducting interviews with the individual and their family/caregiver, and analyzing and interpreting the data collected. Factors such as scheduling conflicts and delays in obtaining necessary information can also affect the overall time frame.
In general, a holistic needs assessment can take from minutes to several hours. Factors that can affect the duration of the assessment include:
- The number of practitioners involved in the assessment process
- The patient’s level of cooperation and engagement
- The availability of relevant medical records and other information
What Are the Benefits of a Holistic Needs Assessment?

A holistic assessment provides a complete picture of the individual’s overall well-being. It can identify underlying issues contributing to a person’s current condition, leading to a more effective treatment plan.
Since the holistic needs assessment emphasizes the patient’s unique experiences, culture, and background, it helps in creating a personalized treatment plan that addresses an individual’s specific concerns. Additionally, it encourages individuals to take an active role in their healing and recovery, which leads to greater self-awareness, self-responsibility, and self-care.
By addressing all aspects of an individual’s well-being, a holistic needs assessment can lead to significant improvement in the following:
- Physical health
- Mental health
- Social and emotional health
A holistic needs assessment is also cost-effective as it addresses everything in one go and can reduce the need for multiple treatments.
Challenges of a Holistic Needs Assessment
A holistic needs assessment includes a comprehensive evaluation of a patient’s medical history, social and economic factors, and lifestyle habits. However, when patients are not forthcoming or have difficulty communicating their needs, accurate data gathering and identification can become challenging. Some other challenges include:
Assessing the patient’s perspective: Holistic needs assessment must consider the patient’s perspective, including their preferences, values, and beliefs, but this can become very challenging if there are language or cultural barriers.
Identifying and addressing social determinants of health: A holistic needs assessment must consider the impact of social determinants, such as poverty, education, and housing, on a patient’s health. Identifying and addressing these factors can be problematic, especially in resource-limited settings.
Time constraints: A holistic needs assessment is a complex and time-consuming process that can be difficult to fit into a busy clinical schedule. Allocating the necessary time and resources to conduct a thorough inspection, especially in understaffed or underfunded healthcare systems, is sometimes difficult to achieve.
The Bottom Line
In conclusion, a holistic needs assessment is a tool for identifying and addressing the diverse needs of individuals, families, and communities. It involves a comprehensive approach to evaluating the physical, emotional, social, and spiritual well-being, as well as the environmental and cultural factors that influence an individual’s overall health. By considering all aspects of the patient’s life, a holistic needs assessment provides the complete picture of their needs and helps to develop more effective interventions and support.
Subscribe to our newsletter for updates!
- Online Experience
- Community Public Health
- Tuition and Financial Aid
The importance of holistic assessment in nursing practice

In traditional health care models, patients are assessed to determine if they have medical problems or diseases. They’re often treated by multiple different health care providers who treat specific issues in isolation. In holistic assessment nursing care, health care providers evaluate a person's overall well-being, including the patient's physical, mental, emotional, and financial situation and their social and living environment. The aim of a holistic nursing assessment is to thoroughly understand all the factors that contribute to a patient’s health so their health care team can develop a comprehensive plan to meet their needs most effectively. 1
This article will cover holistic nursing assessment, including its importance, benefits, and methods.
The importance of holistic assessment in nursing
Holistic health care addresses patients as a whole person, more than merely a conglomeration of systems, vital signs and physical condition. Their psychological or emotional health, physical, social, and spiritual needs all contribute to their well-being. Performing a more comprehensive holistic assessment allows you to fully understand a patient’s circumstances and contributes to better patient care and outcomes. 2
When you ask questions that relate to a patient’s life circumstances, you can create a care plan and effective interventions that address underlying issues in addition to specific symptoms. While a minimal assessment can diagnose that a patient has high blood pressure, a holistic assessment can help you address deeper issues within a person's life. Your patient may be experiencing financial stress and feel like they can only afford cheap, high-sodium, processed food. If you uncover these issues in a holistic assessment, you can help the patient develop a plan to eat well on a budget and learn stress reduction techniques. 2
Tools and techniques for holistic assessment
A holistic nursing assessment includes traditional and nontraditional tools and techniques. While you’ll still be using standard tools to measure physical health, you will also be using assessment forms to interview your patients about various aspects of their lives. You’ll also rely on active listening to understand the intent behind what your patients say and your observational skills to notice issues the patient may not bring up. 2
During an initial holistic health assessment, you’ll ask your patient about any physical problems they have, including a complete review of systems. You’ll also ask about their social and environmental concerns, such as their living conditions, worries, fears, financial concerns, and family issues. Next, ask about your patient’s emotional state and spiritual and religious needs. 3
How technology can support holistic assessments
The digital transformation has changed how society does business and created more convenient and efficient processes in many industries. Health care is no exception. You can take advantage of digital assessment tools, apps, and telemedicine platforms to discover more about your patients’ needs. The rise in wearable technology means your patients can also contribute to their assessment by providing extensive health data from their own devices. They can show you how much activity they get on a daily basis or provide results from continuous glucose monitoring patches. 4
Electronic health records (EHRs) also provide insight into a patient’s medical history, often giving you access to recent evaluations and diagnostic test results. This allows multiple providers to access a single source of truth related to a patient’s care and can eliminate misunderstandings and unnecessary duplicate testing. 5
Integrating holistic assessment into daily nursing practice
Although holistic health assessments can be more time-consuming than performing traditional health assessments, it can help you make informed decisions about patient care that are more targeted and effective. Incorporating core values of holistic nursing and mastering the knowledge and skills you need can help you successfully implement holistic assessments into your daily nursing practice. 6
According to the American Holistic Nurses Association (AHNA), the core values of holistic nursing include: 6
- A holistic healthcare philosophy that includes a commitment to education, reflection, and knowledge
- Ethics grounded in theory and supported by research
- A belief that nurses must care for themselves in order to care for others
- Working with patients to develop shared goals for health and healing
- Embracing assessment and treatment in an environment of caring
The knowledge and skills you need to implement the core values of holistic nursing include the following: 6
- The knowledge necessary to provide quality care in nursing practices
- The expertise needed to make accurate decisions about care and easily perform nursing tasks
- Intuition so you can understand your patients’ experiences and what they’re trying to communicate to you
- An understanding of theories so you can understand, reflect on, and explain practices
- Creativity to develop new approaches to being with your patients and solve problems
Nurses who can prove they have the knowledge and skills to successfully implement these holistic health practices can earn a Holistic Nurse-Certified (HNC) designation through the American Holistic Nurses' Certification Corporation (AHNCC) via a portfolio review and standardized testing. Pursuing a degree with coursework in holistic nursing can also help you learn to incorporate holistic nursing practices in your career. 6
Steps to conducting a holistic assessment in nursing
A holistic assessment is a patient-centered tool for developing a treatment plan based on evidence-based practices, patient values, and nursing intuition. It includes the following steps: 7
- Assessing the patient using critical thinking skills as well as subjective and objective data from various sources
- Reaching a diagnosis to prioritize care based on the fundamental needs of all people
- Planning goals and health outcomes based on evidence-based practices and patient-specific goals
- Implementing the steps in the plan of care
- Evaluating the effectiveness of the patient care plan through reassessment and follow-up
Enhance your holistic nursing skills with an online RN-BSN program
If you’re interested in expanding your nursing practice to include holistic care that meets the optimal health needs of the whole patient and taking on leadership roles in nursing, a Bachelor of Science in Nursing (BSN) Online from Oklahoma City University will help you develop the skills you need. Our renowned faculty are recognized leaders in the field and will help you develop as a health care professional. Plus, our rigorous curriculum covers the evidence-based practices and analytical skills you need to provide patient-centered care. Learn more about admissions requirements or contact one of our admissions outreach advisors today to apply and take the next steps in your rewarding career.
- Retrieved on October 30, 2024, from aiam.edu/alternative-medicine/holistic-assessment-nursing/
- Retrieved on October 30, 2024, from atlashealthmedicalgroup.com/the-ultimate-checklist-for-your-first-holistic-health-assessment/
- Retrieved on October 30, 2024, from cntw.nhs.uk/wp-content/uploads/2019/05/03.-Nursing-Assessment-V02.pdf
- Retrieved on October 30, 2024, from pmc.ncbi.nlm.nih.gov/articles/PMC10350363/
- Retrieved on October 30, 2024, from elationhealth.com/resources/blogs/how-ehrs-enable-better-continuity-of-care
- Retrieved on October 30, 2024, from ojin.nursingworld.org/table-of-contents/volume-6-2001/number-2-may-2001/holistic-nursing-practice/
- Retrieved on October 30, 2024, from ncbi.nlm.nih.gov/books/NBK499937/
Return to Oklahoma City University Online Nursing Blog
Complete the form below before proceeding to the application portal.
Read More from Oklahoma City University Online

Oklahoma City University has engaged Everspring , a leading provider of education and technology services, to support select aspects of program delivery.
What is Holistic Care in Nursing? (With Examples, Principles, & Challenges)

If you have been around nursing or healthcare for any time, you have probably heard the word “holistic” more than a time or two. You may be in nursing school and wondering, “What is holistic care in nursing?” Perhaps you are already a nurse who wants to know how to improve your approach to holistic care. Either way, this article is for you. As you read further, I will tell you about holistic care in nursing. You will learn what it is, why it is important, and find some examples of how to use holistic nursing care. Additionally, I will share some of the challenges you will face in holistic nursing and give you some tips on how to overcome them!
What Exactly is Holistic Care in Nursing?
5 reasons why holistic care is important in nursing, reason #1: holistic nursing embraces the whole person, reason #2: holistic nursing promotes preventive care, reason #3: holistic nursing helps promote self-care, reason #4: holistic care in nursing embraces cultural diversity, reason #5: holistic nursing benefits nurses as well as patients, 5 core principles of holistic nursing, principle #1: holistic philosophy, theories, and ethics, principle #2: holistic caring process, principle #3: holistic communication, therapeutic healing environment, and cultural diversity, principle #4: holistic education and research, principle #5: self-reflection and self-care, what are some good examples of holistic care in nursing, example #1: wellness coaching, example #2: massage therapy, example #3: aromatherapy, example #4: hydrotherapy, example #5: guided imagery, example #6: teaching stress management techniques, example #7: make patient interactions personal, example #8: respecting a patient’s religious beliefs and promoting their right to religious freedom, example #9: providing nutrition advice, example #10: utilizing therapeutic communication, 4 main challenges nurses face in implementing holistic care and how to overcome them, challenge #1: lack of enough education about the holistic care approach, about the challenge:, how to overcome:, challenge #2: getting caregivers involved in patient care, challenge #3: polypharmacy and its effects on patient health, challenge #4: overcoming socioeconomic barriers, my final thoughts, list of sources used for this article.


Holistic Nursing: Integrating Mind, Body, and Spirit in Patient Care
By – James M. Katz, BA
Holistic nursing represents a transformative approach to patient care, integrating mind, body, and spirit to promote overall well-being. This comprehensive healthcare model views patients as whole persons, not just a collection of symptoms or diagnoses. Holistic nurses embrace a philosophy that emphasizes the interconnectedness of physical, emotional, and spiritual health, aiming to provide care that addresses all aspects of a person’s life.
What sets holistic nursing apart is its focus on creating a healing environment and empowering patients to take an active role in their health journey. This approach has gained recognition for its ability to enhance patient outcomes and satisfaction. From conducting holistic assessments to implementing integrative care techniques, holistic nurses play a crucial role in modern healthcare. They use a variety of methods, including mind-body techniques and spiritual care, to support patients’ healing processes and promote long-term wellness.
Key Takeaways
- Holistic nursing treats the whole person, including their body, mind, spirit, and emotions.
- This type of nursing helps patients feel more in control of their health and well-being.
- Holistic nurses use many different methods, including alternative therapies like acupuncture and massage.
- Patient-centered care is a big part of holistic nursing, making patients active participants in their healthcare.
- Holistic nursing can lead to better health outcomes and lower healthcare costs.
Historical Perspective of Holistic Nursing
Early practices.
The roots of holistic nursing trace back thousands of years, with ancient healing traditions recognizing the interconnectedness of mind, body, and spirit. Traditional Chinese Medicine (TCM), originating nearly 5,000 years ago , viewed the human body as a microcosm of interconnected systems, including physical elements and subtle energies like “qi” (life force) and “shen” (spirit) . Similarly, Ayurveda, the ancient medical tradition of India, incorporated beliefs in the five great elements of the universe and the seven primary constituent elements of the body.
In the Western world, Hippocrates, often referred to as the father of medicine, emphasized the healing power of nature in the 4th century B.C. He believed in encouraging the body’s self-healing efforts, an approach that aligns closely with modern holistic nursing principles. This holistic paradigm has been present in healthcare systems across various cultures and can be applied to diverse areas of nursing care, including medical-surgical, mental health, obstetric, pediatric, and public health nursing.
Evolution of the Concept
The concept of holistic care in nursing has evolved significantly over time. Florence Nightingale, considered the founder of both modern and holistic nursing, stressed the importance of nature in the healing process. She taught her students to focus on wellness, unity, and the interrelationship between individuals and their environment. Nightingale’s teachings laid the foundation for what would later become known as holistic nursing.
Throughout the 1700s and into the mid-1900s, nursing was grounded in holistic care principles. Practitioners used various therapeutic approaches, including water therapy, homeopathy, and acupressure, a non-invasive form of acupuncture that has been common in traditional Chinese medicine for the last 3,000 years. Nursing textbooks routinely included medicinal plant theory, emphasizing the importance of considering the whole person in care.
However, the mid-to-late 1900s saw a shift in focus. As technological advancements changed medicine from a service to a for-profit business, many holistic theories were abandoned. The discovery of germs as disease-causing agents led Western medicine to become thoroughly focused on intervention. Diseases were treated as invaders to be destroyed with medicines like penicillin, and physicians paid less attention to healthy lifestyle choices, environmental factors, and emotional health.
Modern Interpretations
The limitations of the purely interventional approach became clear by the late 20th century. Some scientific medical cures proved more harmful than the diseases they sought to treat, while other diseases and chronic conditions failed to respond to scientific treatment. This realization led to a renewed interest in holistic health education in the West.
In 1975, the first National Conference on Holistic Health was conducted in California, marking a significant milestone in the revival of holistic practices . Soon after, the American Holistic Health Association (AHHA) and the Holistic Medical Association were formed, further solidifying the place of holistic approaches in modern healthcare.
The American Holistic Nurses Association (AHNA) was founded in 1980 to serve as a voice for holistic nurses and to promote education in the philosophy, practice, and research of holistic caring and healing . In 1997, the American Holistic Nurses Certification Corporation (AHNCC) was established to credential holistic nurses, further legitimizing the field.

The Five Core Values of Holistic Nursing
Holistic nursing is grounded in a comprehensive approach to patient care that integrates the mind, body, and spirit. The American Holistic Nurses Association (AHNA) has established five core values that form the foundation of holistic nursing practice. These values guide nurses in providing compassionate, patient-centered care that addresses the whole person.
Holistic Philosophy and Education
The first core value emphasizes the importance of a holistic philosophy and ongoing education . Holistic nursing is based on a philosophical framework that embraces holism and a commitment to continuous learning. This approach recognizes that for human beings, the whole is greater than the sum of its parts, acknowledging the interdependence of biological, social, psychological, and spiritual aspects. Holistic nurses are encouraged to seek and acquire knowledge and skills pertinent to their practice, maintaining professional records that provide evidence of competency and lifelong learning.
Holistic Ethics, Theories, and Research
The second core value underscores the significance of ethics, nursing theories, and research in guiding holistic nursing practice. Holistic nurses are expected to practice within the profession’s ethical code and use current knowledge, including research findings, to expand their clinical practice and professional performance. The AHNA supports both quantitative and qualitative research to expand the body of knowledge in holistic nursing . This core value emphasizes that professional nursing is grounded in theory, informed by research, and bound by ethical principles to ensure competent and principled practice.
Holistic Nurse Self-Care
Self-care is a crucial aspect of holistic nursing. This core value recognizes that to facilitate healing in others, nurses must first undertake healing within themselves. Holistic nurses are encouraged to engage in various self-care practices, including mind-body techniques, good nutrition, exercise, and lifelong learning. Regular mindfulness practices and meditation have been shown to increase compassion and decrease burnout among nurses . By valuing and practicing self-care, holistic nurses can effectively manage physical and emotional stressors, becoming more effective caregivers and healers.
Holistic Communication and Environment
The fourth core value focuses on holistic communication, creating a therapeutic environment, and cultural competence. This value emphasizes the importance of engaging with clients to promote mutually-determined goals for health and healing. Holistic care respects human dignity and is based on a relationship of respect, relative openness, equality, and mutuality between healthcare providers and patients. Holistic nurses are expected to possess knowledge of cultural traditions and use this understanding to provide culturally competent care.
Holistic Caring Process
The final core value centers on the holistic caring process, which is an evolution of the traditional nursing process. This approach emphasizes assessment and therapeutic care that addresses client patterns, problems, and needs in an atmosphere of caring. Holistic nurses recognize the complex dynamic relationship between health, illness, and wellness, and value healing as a central component of their practice. They act as guides in the healing process, protecting patient dignity and recognizing that the patient is the authority on their own health experience.
By adhering to these five core values, holistic nurses can provide comprehensive care that goes beyond treating physical symptoms. This approach has been shown to improve patient satisfaction, increase the depth of care providers’ understanding of patients and their needs, and enhance patients’ self-awareness and self-confidence. As the healthcare landscape continues to evolve, these core values serve as a guiding framework for nurses committed to providing holistic, patient-centered care.
Assessing Patients Holistically
Holistic assessment in nursing is a comprehensive approach to evaluating a patient’s overall health and well-being. It goes beyond traditional methods by considering various aspects that may impact a person’s health , including physical, mental, social, financial, and environmental factors . This approach aligns with the philosophy of holistic nursing, which aims to heal the whole person.
Physical Assessment
The physical assessment is a crucial component of holistic nursing. It examines an individual’s overall physical condition, including any medical conditions, medications being taken, and physical limitations that may affect daily activities. Nurses conduct thorough physical examinations and may use diagnostic tests to gather comprehensive information about the patient’s health status.
During this assessment, nurses also evaluate the patient’s lifestyle choices and habits, such as exercise, nutrition, and sleep patterns. This information helps create a more complete picture of the patient’s physical health and identifies areas for potential improvement.
Psychological Evaluation
A holistic assessment includes a thorough evaluation of the patient’s mental and emotional well-being. This involves assessing the patient’s psychological status, including any mental health conditions or disorders . Nurses may use various tools and techniques to gather information about the patient’s emotional state, cognitive functioning, and overall mental health.
The psychological evaluation also considers the patient’s social support network and living conditions, as these factors can significantly impact mental health. By understanding the patient’s psychological state, nurses can better address their emotional needs and provide appropriate support or referrals for mental health services.
Spiritual and Cultural Considerations
Spiritual and cultural aspects are integral to holistic nursing assessments. Nurses recognize the importance of spiritual comfort and aim to respond to all patients’ spiritual needs, regardless of their religious beliefs. This approach is consistent with the ethical codes of professional nursing organizations and the International Council of Nurses. When assessing spiritual needs, nurses consider the patient’s beliefs, values, and cultural background. They may inquire about the patient’s spiritual practices, sources of meaning and purpose, and any spiritual concerns related to their health condition. This information helps nurses provide culturally competent care and address the patient’s spiritual needs as part of their overall treatment plan.
It’s important to note that spirituality is often viewed in broad terms and is not necessarily connected to organized religion. Nurses should be prepared to engage with patients from diverse spiritual backgrounds and respect their individual beliefs and practices.
The holistic assessment process emphasizes person-centered care and mutual goal-setting. Instead of focusing solely on the most acute medical issue, nurses engage in extensive conversations with patients, covering various aspects of their lives. This collaborative approach allows nurses and patients to work together to establish wellness goals and determine the best strategies for achieving them.
By conducting holistic assessments, nurses can gain a deeper understanding of their patients’ unique challenges, strengths, and goals. This comprehensive approach has several benefits, including increased communication between nurses and patients, improved patient satisfaction, and potentially better health outcomes. Patients often feel more valued and engaged in their care when their beliefs and values are respected, and they are encouraged to actively participate in crafting their care plans.
However, it’s worth noting that implementing holistic assessments can be challenging. Nurses may face time constraints, lack of training, or uncertainty about their role in providing spiritual care. Additionally, cultural and religious differences between nurses and patients may affect the ability to provide comprehensive spiritual care. Despite these challenges, the growing emphasis on holistic care in nursing underscores the importance of addressing patients’ physical, psychological, and spiritual needs for optimal health outcomes.
The Importance of Holistic Nursing in Healthcare
Patient empowerment.
Holistic nursing helps patients take charge of their own health. By looking at the whole person, not just their illness, nurses can guide patients to make better lifestyle choices. This makes patients feel more in control and involved in their care. When patients understand their health better, they are more likely to follow treatment plans and manage their conditions effectively.
Improved Health Outcomes
When nurses consider a patient’s physical, emotional, and spiritual needs, the care they provide is more complete. This approach can lead to better health results. Patients who feel understood and supported are more likely to stick with their treatments and see improvements in their health. Holistic nursing also helps in preventing and managing long-term illnesses like heart disease and diabetes.
Stress and Emotional Well-being
Stress and emotions play a big role in a person’s health. Holistic nurses know this and work to help patients manage stress and improve their emotional well-being. By addressing these factors, nurses can help reduce the risk of chronic diseases and improve overall health. This kind of care makes patients feel more balanced and less anxious, which is good for their overall well-being.
Implementing Holistic Care Plans
Implementing holistic care plans is a comprehensive approach that considers the physical, mental, emotional, and social aspects of a patient’s well-being. This method aligns with the World Health Organization’s definition of health as “a state of physical, mental, and social well-being and not merely the absence of disease or infirmity” . Holistic care plans are particularly crucial in an aging society with limited economic resources, where integrated support for individuals with chronic or long-term conditions is essential.
Goal Setting
Setting health goals is a fundamental component of a holistic care plan. Goals provide patients with clear direction, motivation, and a sense of purpose. When establishing wellness goals, it’s important to consider various aspects of health, including nutrition, exercise, sleep, stress management, and mental well-being. This ensures a balanced approach to overall wellness.

Collaborative Approach
Holistic care plans necessitate collaboration between various stakeholders, including healthcare professionals, social care providers, patients, and their families. This collaborative approach is crucial, especially for older adults who often face complex, interrelated problems encompassing physical, psychological, and social health. The American Nursing Association (ANA) defines holistic care as an integration of body, mind, emotion, spirit, sexual, cultural, social, energetic, and environmental principles and modalities to promote health, increase well-being, and actualize human potential. This definition underscores the need for a multidisciplinary approach in implementing holistic care plans.
Collaboration in healthcare settings, whether in an emergency room or a public health setting, is essential. Public health initiatives often require an even higher level of collaboration due to the broad scope of healthcare initiatives they encompass. The complexity of community health challenges necessitates more than traditional healthcare delivery models, considering factors such as social determinants of health (SDOH).
Personalized Interventions
Personalized interventions are a key aspect of holistic care plans. The ‘Partnering in Healthcare’ framework emphasizes understanding the whole person (or family), including their physical, cultural, and social context, as well as differences in health, wellbeing, and safety. This approach involves putting people and families at the center of care, providing emotional support and empathy, involving family and friends, and showing compassion and respect.
Specific, measurable actions associated with personalized care include building relationships through active listening, expressing caring and empathy, and personalizing care practices such as including family, knowing the patient, and eliciting and respecting patients’ values. These personalized interventions contribute to improved patient satisfaction and enhanced quality of care.
Implementing holistic care plans requires consistent monitoring and adaptation. As patients work toward their wellness goals, it’s essential to be prepared to adjust the plan as needed. Life is dynamic, and a holistic care plan should be flexible enough to evolve with changing circumstances. Regular progress assessments help patients stay on track and allow for necessary adjustments to the care plan.
By implementing comprehensive, collaborative, and personalized holistic care plans, healthcare providers can enhance patient outcomes, improve quality of life, and potentially reduce healthcare costs by preventing complications and shortening hospital stays.
Mind-Body Techniques in Holistic Nursing
Meditation and mindfulness.
Meditation and mindfulness practices have gained significant popularity in holistic nursing due to their numerous health benefits. These ancient techniques, rooted in Eastern traditions, focus on mind-body integration and are used to calm the mind and enhance overall well-being. Meditation involves maintaining mental focus on a particular sensation, such as breathing, a sound, or a visual image, while mindfulness emphasizes maintaining attention on the present moment without judgment.
The prevalence of meditation practice among U.S. adults has more than doubled between 2002 and 2022, from 7.5% to 17.3% . This increase in popularity is likely due to the growing body of evidence supporting its effectiveness in managing various health conditions. Studies have shown that meditation and mindfulness practices can help reduce symptoms of anxiety, depression, and stress. They have also been found to be effective in managing chronic pain, improving sleep quality, and enhancing cognitive function.
In holistic nursing, meditation and mindfulness techniques are often incorporated into patient care to promote relaxation, reduce stress, and improve overall well-being. These practices can be particularly beneficial for patients dealing with chronic conditions, cancer, or mental health issues.
Guided Imagery
Guided imagery is a mind-body-spiritual technique that directs one’s imagination toward a relaxed, positive state to promote health. In this practice, a holistic nurse uses spontaneous speech or follows a script to guide the patient’s imagination, creating positive mental images that aid in relaxation, stress reduction, and a sense of empowerment.
Research has shown that guided imagery can have powerful effects in various healthcare settings. Studies have found significant decreases in systolic blood pressure, pulse rate, and perceived stress levels among healthcare workers after guided imagery sessions. In nursing practice, guided imagery has been used to reduce patients’ anxiety before invasive procedures and decrease postoperative pain.
A systematic review of relaxation, meditation, and guided imagery techniques found that these strategies reduced physical discomfort and improved quality of life in patients with heart failure. Participants experienced less dyspnea and fewer sleep disturbances compared to those receiving typical medical care.
Biofeedback
Biofeedback is an alternative medicine approach that teaches individuals to change the way their body functions. It is a mind-body therapy that may improve physical and mental health by providing real-time feedback on physiological functions such as heart rate, breathing, and muscle tension.
During a biofeedback session, a healthcare provider uses noninvasive monitoring equipment to measure involuntary bodily functions. Based on the feedback from these instruments, the provider suggests ways for the patient to create voluntary changes in these functions. With practice, patients can learn to make these bodily changes without equipment.
Biofeedback can be particularly useful in managing symptoms of certain conditions. It has shown efficacy in relieving pain and anxiety, making it a valuable tool in stress reduction. A study conducted in the emergency department confirmed that biofeedback was easily adaptable to various environments.
In holistic nursing practice, biofeedback can be used to help patients manage various health issues, including chronic pain, headaches, and stress-related conditions. By learning to control certain physiological processes, patients can gain a sense of empowerment and take an active role in their healing process.
Spiritual Care in Holistic Nursing
Spiritual care is an essential component of holistic nursing, addressing the patient’s search for meaning and purpose in life. It goes beyond physical manipulation or pharmaceutical medication, extending into a person’s environment, emotions, and spiritual health. Spirituality encompasses a sense of connection to something greater than oneself and typically involves a search for meaning and purpose in life.
Addressing Spiritual Needs
Nurses play a crucial role in assessing, diagnosing, and responding to the spiritual needs of each patient and their significant others. To provide effective spiritual care, nurses need to conduct spiritual assessments, recognize the difference between religious and spiritual needs, and identify appropriate interventions. Spiritual assessments involve asking patients open-ended questions to evaluate their spiritual needs. Nurses can incorporate these identified needs into the patient’s care plan, using relationships, therapeutic communication, and physical therapeutic interventions.
Spiritual care interventions can take various forms, including:
1. Praying with or for the patient 2. Offering a supportive presence 3. Facilitating the practice of the patient’s religion 4. Exploring alternatives to challenges 5. Promoting forgiveness 6. Assisting patients in exploring realistic expectations of themselves 7. Promoting deeper expression of feelings and emotions through therapeutic communication
Cultural Competence
Cultural competence is crucial in providing spiritual care, as it allows nurses to effectively interact with people from different cultural backgrounds. It involves understanding and appreciating various cultural, racial, ethnic, gender, and sexual identities.
To develop cultural competence, nurses should: 1. Be aware of their own cultural worldview 2. Maintain a positive attitude toward cultural differences 3. Continuously improve their knowledge of different cultural practices and worldviews 4. Develop cross-cultural skills
Establishing common ground is vital in culturally competent spiritual care. Nurses can share their own experiences and work in diverse environments to foster a sense of belonging. Learning new languages can help address language gaps in healthcare, which often negatively impact patient outcomes and satisfaction.
End-of-Life Care
Spiritual care is particularly important in end-of-life situations, where patients and their families often experience spiritual distress. Hospice and palliative care nurses providing spiritual care have reported lower stress levels and reduced burnout.
In end-of-life care, nurses can help patients find hope, meaning, and inner peace through various interventions:
1. Promoting physical relaxation 2. Enhancing self-awareness 3. Facilitating a greater sense of connection with others 4. Encouraging forgiveness 5. Fostering a more cooperative attitude
These interventions can lead to increased physical healing, pain reduction, and personal growth.
Many healthcare facilities employ professionally trained chaplains to assist with the spiritual, religious, and emotional needs of patients, family members, and staff. Chaplains can meet with individuals regardless of their belief systems and can be instrumental in reducing anxiety and distress.
By addressing patients’ spiritual needs, nurses can improve health outcomes, quality of life, and help patients cope with the stress and suffering associated with serious illness and end-of-life experiences . Through therapeutic presence, unconditional acceptance, and compassion, nurses provide spiritual care that helps patients find hope and meaning in their life experiences.
Measuring Outcomes in Holistic Nursing
Measuring outcomes in holistic nursing is essential for evaluating the effectiveness of care and improving patient well-being. This process involves assessing various aspects of a patient’s health, including physical, mental, emotional, and spiritual dimensions. By utilizing comprehensive assessment tools and focusing on patient-centered outcomes, holistic nurses can gain valuable insights into the impact of their interventions.
Quality of Life Indicators
Quality of life is a crucial aspect of holistic nursing care. The World Health Organization defines quality of life as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns”. To measure this multifaceted concept, the WHOQOL Group developed the WHOQOL assessment, which aims to evaluate quality of life across different cultures .
Quality of life indicators in holistic nursing often encompass:
1. Physical health and functioning 2. Psychological well-being 3. Social relationships 4. Environmental factors 5. Spiritual and existential aspects
These indicators provide a comprehensive view of a patient’s overall well-being and can help guide interventions and care planning.
Patient Satisfaction
Patient satisfaction is another crucial outcome measure in holistic nursing. It reflects the extent to which patients feel their needs and expectations have been met during their care experience. A study conducted in Saudi Arabia found that cancer patients’ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7219452/ satisfaction with holistic care approach was a good measurement of the quality of care.
The study revealed that patients’ satisfaction with holistic care ranged from very satisfied to satisfied across four aspects:
1. Physical care 2. Emotional support 3. Social assistance 4. Spiritual care
Interestingly, the study found significant differences in satisfaction levels for social and spiritual aspects when grouped by age, with a p-value of 0.001. This highlights the importance of tailoring holistic care approaches to different age groups and considering cultural factors in patient satisfaction.
Holistic Health Assessments
Holistic health assessments are comprehensive tools used to evaluate a patient’s overall well-being. These assessments consider various aspects of health, including physical, mental, social, and spiritual dimensions. The Holistic Health Assessment Tool for dialysis patients (HHAT-D) is an example of such an instrument developed to assess the holistic health status of patients on maintenance hemodialysis.
The HHAT-D evaluates:
1. Anthropometric measurements 2. Biochemical parameters 3. Functional status 4. Psychological status 5. Dietary intake 6. Coping strategies
In a study using the HHAT-D, researchers found that 73.3% of patients were mild to moderately malnourished . The tool showed a highly significant negative correlation between anthropometric measurements and HHAT-D scores (p<0.01), confirming its validity in assessing the degree of malnutrition.
Another example is the Holistic Health Status Questionnaire (HHSQ), which was developed to assess the holistic well-being of Chinese individuals with chronic diseases. This tool focuses on the interconnectedness of bio-psycho-social-spiritual dimensions and incorporates cultural attributes specific to Chinese populations.
By utilizing these comprehensive assessment tools, holistic nurses can gain a more complete understanding of their patients’ health status and tailor interventions accordingly. These assessments not only help in identifying areas of concern but also in tracking progress over time, ultimately leading to improved patient outcomes and quality of life.
Roles and Responsibilities of Holistic Nurses
Patient interaction and communication.
Holistic nurses focus on building strong relationships with their patients. They make sure to learn each patient’s name, maintain eye contact, and show genuine compassion. This approach helps patients feel more comfortable and involved in their own healing process. By using techniques like imagery and relaxation, holistic nurses aim to reduce pain and stress without always relying on medication.
Assessment and Care Planning
Holistic nurses assess patients by considering their physical, emotional, and spiritual needs. They look at the whole person, not just the symptoms. This means they ask questions about lifestyle, diet, and even stress factors that might affect health. By understanding the complete picture, holistic nurses can create personalized care plans that address all aspects of a patient’s well-being.
Use of Alternative Therapies
In addition to traditional medical treatments, holistic nurses often use alternative therapies. These can include practices like massage, acupuncture, and meditation. Combining these methods with conventional medicine can offer a more comprehensive approach to healing. Holistic nurses are trained to know when and how to use these therapies to best support their patients’ overall health.
Challenges and Opportunities in Holistic Nursing
Integration with traditional medicine.

Regulatory and Legal Considerations
Holistic nurses must navigate a complex landscape of regulations and legal issues. Different states and countries have varying rules about what holistic practices are allowed. This can make it hard for nurses to know what they can and cannot do. Staying informed about these regulations is crucial for safe and effective practice.
Future Trends and Innovations
The field of holistic nursing is always evolving. New techniques and treatments are constantly being developed. This offers exciting opportunities for nurses to expand their skills and improve patient care. Keeping up with these trends can be challenging but also very rewarding. The future of holistic nursing looks bright, with many chances for growth and innovation.
Holistic nursing has a profound influence on patient care, integrating physical, mental, and spiritual aspects to promote overall well-being. This approach goes beyond treating symptoms, aiming to heal the whole person. By embracing core values like self-care, cultural competence, and a comprehensive caring process, holistic nurses create an environment that fosters healing and empowers patients to take an active role in their health journey. The implementation of holistic care plans and mind-body techniques further enhances the effectiveness of this patient-centered approach.
To sum up, the field of holistic nursing continues to evolve, with a growing emphasis on measuring outcomes and improving patient satisfaction. By using comprehensive assessment tools and focusing on quality-of-life indicators, holistic nurses can fine-tune their interventions and provide more effective care. As healthcare faces new challenges, the holistic approach offers a promising path to enhance patient outcomes, increase satisfaction, and promote long-term wellness. This practice not only benefits patients but also contributes to the professional growth and job satisfaction of nurses themselves.
Thinking of becoming a Holistic Healthcare Specialist? The American Institute of Health Care Professionals offers an excellent online holistic healthcare certification program available to license nurses (RNs). The program also requires completion of 5 online holistic nursing courses. For more information on this Holistic and Integrative Healthcare Specialist program please visit our main page
- What is holistic nursing? Holistic nursing is a type of nursing that focuses on healing the whole person. This means looking at a patient’s physical, emotional, spiritual, and social needs, not just their illness or symptoms.
- Why is holistic nursing important in healthcare? Holistic nursing is important because it helps patients feel more in control of their health. By looking at the whole person, nurses can help improve overall health outcomes and address issues like stress and emotional well-being.
- What practices do holistic nurses use? Holistic nurses use a variety of practices, including patient-centered care, complementary and alternative therapies like acupuncture and massage, and techniques that integrate mind, body, and spirit.
- What are the roles and responsibilities of holistic nurses? Holistic nurses interact closely with patients, create personalized care plans, and often use alternative therapies. They focus on understanding the whole patient and helping them take an active role in their own care.
- How can one become a holistic nurse? To become a holistic nurse, you need to have the required knowledge and skills, complete a certification program, and engage in continuing education to stay updated on holistic practices.
- What challenges do holistic nurses face? Holistic nurses may face challenges like integrating their practices with traditional medicine, dealing with regulatory and legal issues, and staying updated with future trends and innovations in healthcare.
- What are the main principles of holistic nursing? The five main principles of holistic nursing encompass holistic philosophy, theory, and ethics; the holistic caring process; holistic communication, therapeutic environment, and cultural diversity; holistic education and research; and holistic nurse self-care.
- What are the four domains of holistic care in nursing? Holistic care in nursing is guided by a philosophy derived from humanism and holism, focusing on mutual understanding of a patient’s physical, psychological, emotional, and spiritual dimensions.
- Can you explain the holistic approach to patient care? The holistic approach to patient care involves treating the entire person, addressing physical, mental, spiritual, and social needs. This method is based on the understanding that all these aspects are interconnected and impact overall health, with imbalances in one area potentially affecting others.
- What does the third core value of holistic nursing, the holistic caring process, entail? The third core value, Holistic Nurse Self-care, emphasizes the importance of nurses engaging in self-care. This practice is crucial as it helps nurses promote health and personal awareness, enabling them to better serve and heal others.
Research Articles:
[Retracted] Benefits and Barriers of Holistic Nursing Training by High-Fidelity Simulation in Obstetrics. Wenxi Zhang, Et Al. Computational and Mathematical Methods in Medicine First published: 28 June 2022
Access link here
Factors Influencing Provision of Holistic Nursing Care to Patients Admitted in Medical Wards at Kenyatta National Hospital, Kenya. Khasoha, Inyama Et Al.(2020) Asian Journal of Research in Nursing and Health, 3 (2). pp. 20-35.
Holistic Nursing in Practice: Mindfulness-Based Yoga as an Intervention to Manage Stress and Burnout. Hilcove K, Et Al. Journal of Holistic Nursing. 2021;39(1):29-42.
Phenomenology for the Holistic Nurse Researcher: Underpinnings of Descriptive and Interpretive Traditions. Patton CM. Journal of Holistic Nursing. 2020;38(3):278-286.
The nursing process, holistic assessment and baseline observations
Pauline Hamilton and Theresa E. Price
Learning outcomes
This chapter will help you:
• Identify the stages of the nursing process and discuss the value of using a problem-solving approach to care
• Discuss how the use of a model of nursing can enhance patient/client care
• Explore the approaches to nursing care used in different settings
• Identify the need for careful documentation as part of nursing practice
• Discuss different nursing assessment strategies
• Explain how body core temperature is assessed using tympanic, oral, axillary and rectal routes, and with different types of thermometer
• Accurately assess and record adults' and children's temperature, pulse, blood pressure, respirations, Early Warning Scores, height, growth and weight, with reference to normal values
• Explain the nursing interventions used to manage pyrexia and hypothermia.
Introduction
This chapter provides an introduction to the nursing process and how it can be applied to different individuals who have varied healthcare needs. It acknowledges the diversity of nursing and provides examples of how the nursing process can be applied in child, mental health, learning disability and adult settings.
The key nursing skills required for holistic assessment are included, with emphasis on the need for effective verbal and written communication skills to promote accurate assessment, followed by effective nursing intervention. Tools that assist in the assessment of individuals are explored, as well as some models of nursing and approaches to care planning.
Assessment of a person's health status includes the measurement of four vital signs: body temperature, blood pressure, pulse and respirations. In addition, a person's weight, height and, in children, the growth rate may be measured. This chapter explains how each of the vital signs is measured and recorded and, for patients who are acutely ill, entered into an Early Warning Score chart (EWS). Assessment of health status usually takes place:
• When a person is admitted to a healthcare system
• If there is a change in health status
• To monitor change as a result of treatment, e.g. administration of medication
• Before, during and after surgery.
The nursing process
Nursing and healthcare delivery systems throughout all fields of nursing are diverse. The philosophies that underpin approaches to nursing vary enormously. In the past, the medical model was prevalent in many areas of nursing. Using this approach, nursing care usually followed the medical diagnosis and was focused on the physical condition of the person. The practice of nursing is based on interpersonal relationships (see Ch. 9 ), with other technical aspects of nursing following.
In recent years, there has been a move away from the medical model, recognizing the individuality of patients/clients and the need to address issues that go beyond the scope of physical care and medical diagnosis. However, medical diagnosis not only affects the needs that people may have, but also has an impact on other aspects of life. Thus, there is an attempt to provide holistic care to all groups of people requiring support from nurses and other healthcare professionals. There is also an increasing body of nursing knowledge available to support different nursing strategies and approaches to care, i.e. evidence-based practice (see Ch. 5 ). This too has an impact on care given. The decision to utilize a particular approach to care should therefore be based upon the unique needs of the person and family, as well as the nursing context ( Department of Health, DH 2010a ).
Yura and Walsh first described the nursing process in 1967 as a means of adopting a problem-solving approach to nursing care. The nursing process provides a systematic way of examining people's problems with a view to providing interventions that would move towards resolving the problems. Their view was that nursing comprises more than intuitive care and that a systematic approach would allow further analysis of the problems that people present with and how they might be resolved. It should be noted that problems identified are problems of the person, not nursing problems. Thus, management of these problems should be person centred ( Yura & Walsh 1967 ).
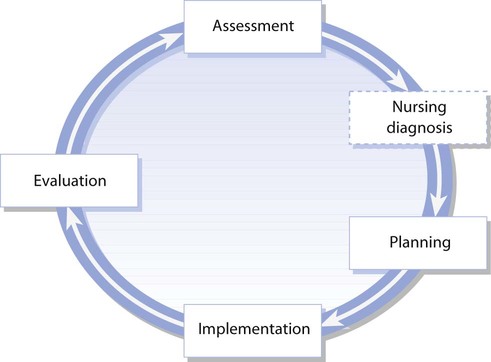
The nursing process can be applied in all nursing settings although the way in which it is applied depends on the health needs of patients/clients, the skills of the nurses and the care environment. The nursing process is cyclical and has a number of stages:
• Identify with the person what the problems are – assessment
• Make plans to address the problems – planning
• Take steps to manage the problems – implementation
• Reflect on what has happened – evaluation.
Sometimes a fifth stage is added to the nursing process – the nursing diagnosis stage – which fits between the stages of assessment and planning ( Fig. 14.1 ). The nursing diagnosis stage has been adopted more in North America than in the UK. The North American Nurses Diagnosis Association (NANDA) has provided standardized nursing diagnoses for many situations ( NANDA 2008 ). Nursing diagnosis explains the effect of the medical diagnosis. For example, the patient may have suffered a heart attack (myocardial infarction) and so one of the nursing diagnoses may be ‘central chest pain’. Nursing diagnosis has been used to standardize terminology and assist the process of audit, a mechanism to measure quality of care to determine if standards are being met.
The nursing diagnosis stage relates to the diagnosis of nursing issues, which may be based on an underlying medical condition but differs from the medical diagnosis. Medical diagnosis is the identification of disease from examination of symptoms and presenting features, whereas nursing diagnosis is more about gaining understanding of the person's situation, which may have wider implications for the person and also impact on other healthcare professionals ( Barker 2009 ; NANDA 2008 ). The approach to planning care influences whether or not the nursing diagnosis stage is included. Patterns of care delivery vary and the UK is moving towards multidisciplinary ways of working, with documentation being designed to incorporate multidisciplinary terminology.
As the nursing process is cyclical in nature, evaluation can lead to reassessment if required. If patient/client goals (see p. 310 ) have been achieved, care can be stopped relative to the goal, or the plan of care may be modified if the goal has not been fully achieved.
While the nursing process can be applied in different settings, it is helpful to use a tool that will provide further guidance appropriate to the needs of people and the care setting. This can be achieved by the use of a model of nursing (see p. 311 ). The stages of the nursing process are explored below.
The first stage is assessment of the patient's/client's and family's needs. Assessment involves collecting information (data) about the person and using that information to make decisions about what care, support or intervention is required. Decision-making involves organizing and interpreting the information collected. Professional judgement may also contribute towards the decision-making process. Assessment documentation and techniques vary according to the setting, e.g. outpatient, inpatient, short stay, ambulatory care, rehabilitation, day care, primary care based in the home, clinics or surgeries. Risk assessment is discussed fully in Chapter 13 ; however, it is an integral part of the assessment process.
As assessment is the cornerstone of establishing what a person's needs are, so the quality of assessment is pivotal to the success of the nursing process. Successful nursing intervention hinges on a complete and thorough assessment being undertaken. Even throughout the other stages of the nursing process, the nurse continues to assess the response to care and success of interventions. Thus assessment is an ongoing process. The aims of assessment are to:
• Determine the needs and potential needs of the person and their family
• Gather information on which a plan of care may be based
• Document information that will provide a basis for reassessment and evaluation
• Act as a mechanism for quality care
• Fulfil statutory obligations
• Aid the structure of nursing knowledge.
Best practice in assessing, planning and implementing care can be achieved by incorporating principles from The Department of Health Essence of Care 2010: Benchmarks for Self Care into the process of assessment. The document advocates that healthcare workers seek the views of the person to inform the care plan ( DH 2010b ).
Assessment is a complex, time-consuming activity that requires many skills. Assessment of someone's needs should be performed jointly with the person whenever possible. Establishing people's own perspective of their problems helps to create partnership working and assists in providing person-centred care that is holistic in nature. Sometimes, this is not possible due to the nature of the person's problems, e.g. in a high-dependency setting when the patient is unconscious, or in a mental health assessment unit when a client is confused and disorientated.
The information required in any given assessment situation will be determined by the nursing context. Confidentiality must be maintained in all settings ( Nursing and Midwifery Council, NMC 2008 ; see also Ch. 7 ). Information should be collected systematically to ensure that important issues are not overlooked. A combination of observation, interview and measurement is required to provide a full assessment ( NANDA 2008 ).
Observation is a key nursing skill that informs the overall assessment process. Observing is a form of data collection made by using the senses. Visual observation can relate to all aspects of the person. Someone's general appearance and physical signs such as skin condition can be observed (see Ch. 16 ). Touch is also used to assess characteristics such as the temperature of a person's skin, presence or absence of pulses or signs of dehydration such as dry, inelastic skin ( Barker 2009 ). Smell can be used to assess dimensions of a person in relation to the environment, such as chemicals in the air. In relation to the person, alcohol may be smelt on their breath or smoke on their clothes.
Interactions with other people can be observed, e.g. verbal and non-verbal communication (see Ch. 9 ). People's behaviour can also be observed, e.g. their reactions to a particular situation, including emotional signs such as crying. Observations should be systematic to maximize the information gathered.
To complete assessment accurately, practitioners should strive for objectivity. Personal interpretations of observations should be avoided. For instance, when describing a person's physical characteristics, it is desirable to retain objectivity and, where possible, to be specific. For example, blood pressure ‘180/95’ instead of ‘blood pressure high’, or ‘smiles frequently’ rather than ‘happy’. Essential nursing skills include objective measurement. Equipment is often used, such as a thermometer to measure temperature ( p. 323 ) or a sphygmomanometer to measure blood pressure ( p. 328 ). Height and weight may be measured with the use of a measuring tape and set of scales ( p. 334 ). Quantifiable information is therefore acquired through the use of equipment as well as direct observation.
Information can be collected in a variety of ways, depending on the situation. The initial assessment of people attending an emergency department will differ greatly from the assessment undertaken by a practice nurse who is immunizing a family going abroad on holiday. The practice nurse makes an assessment of what is required for the safety of the travellers in the longer term, whereas the emergency department nurse makes an initial short-term assessment of the person in relation to their priority for treatment.
Holistic assessment
For assessment to be comprehensive, it should be undertaken in a holistic manner. Thus, the following dimensions of need should be assessed ( Fawcett 2005 ):
• Physical
• Sociocultural
• Spiritual
• Psychological
• Emotional.
While people may present to the nurse with similar medical or social problems, it is only by thorough and systematic assessment that includes the physical, psychological, sociocultural, spiritual and emotional dimensions of their lives that a truly individualized plan of care can be developed. It can, however, be difficult to separate the dimensions, as they are all interrelated and can impact on a person's health in different ways ( Box 14.1 ).
Anna is a young married woman with small children who is undergoing radiotherapy treatment for cancer. She may experience physical side-effects, including fatigue. The fatigue may cause anxiety, as Anna may be less able to look after her children and fulfil family obligations. She may consider not completing the course of radiotherapy to allow the fatigue to diminish. It is only by undertaking a holistic assessment that the impact of the treatment on Anna and her family's lives can be ascertained.
Student activities
• Think about the dimensions of holistic care and try to identify more aspects of Anna's life that may be affected.
• Assuming that Anna's children had left home and the other circumstances were unchanged, identify the potential differences that Anna and her children may face.
• Discuss your ideas with a colleague.
The nurse's role is to identify and react to a person's response to their own situation. Thus, while a medical condition is acknowledged when assessing a patient or client, it only forms part of the assessment. The aim is to acquire the fullest information necessary without gathering irrelevant information.
Priorities of assessment may differ within different fields of nursing. In mental health, assessment may concentrate initially on psychological and social dimensions, since much of the care of people with mental health problems centres on human responses to illness (see p. 316 ). With children, it is appropriate to use a child and family-centred approach (see p. 317 ). The benefit of such an approach is that it addresses the needs of the family as well as the child. Learning disability assessment also has unique characteristics, which are discussed later. Nurses working in many settings will meet people with a learning disability as most live in the community and access health services in the usual ways, e.g. though primary care via their GP or practice nurse. What is important is that the principles discussed on page 315 are incorporated into the assessment process.
The nurse will undertake a decision-making process to make sense of the data collected from the assessment and formulate a plan of care. Thus the nurse's assessment of the patient/client will form the nursing history.
Sources of information
Information can be gathered for assessment purposes from:
• The patient/client – the primary source
• Other people or records – secondary sources.
Primary source
The patient or client should be the primary source of information, including children and young people as developmentally appropriate, as it is important to elicit their own perspective of their situation. To successfully interview the patient/client, the nurse needs to be a skilled communicator; questioning, actively listening and eliciting information (see Ch. 9 ). The nurse's questioning technique will depend on the circumstances. Open questions are often appropriate to encourage the person to respond, however there are times when it is more appropriate to use closed questions, e.g. in the case of an acutely ill breathless patient or a patient in extreme pain.
Questions for the nurse to ask during the assessment interview should be holistic. Factors that encompass an holistic perspective may relate to physical, sociocultural, spiritual, psychological and emotional factors. It is important for the nurse to be aware of factors that may influence the patient or client's situation. Therefore, consideration of these five factors may assist the nurse in formulating appropriate questions to ask the patient or client. Perhaps environmental factors influence the person with asthma and it would be appropriate to ask about the nature of their workplace. An example of how these factors can be incorporated into holistic assessment of breathing can be seen in Box 14.2 .
Box 14.2 Nursing considerations as part of holistic assessment of breathing
1. Physical:
• What is the rate and pattern of breathing?
• Is breathing affected by activities or environmental factors?
2. Psychological:
• Is there a need for breathing or relaxation exercises?
• Is there a chance that emotion may affect breathing?
3. Sociocultural:
• Are there influences on the person's behaviour, e.g. smoking?
• What are the person's health beliefs (see Ch. 1 ) about coughing, expectorating or using inhaled medication?
4. Environmental:
• Are there factors influencing breathing, e.g. medication, position in bed, home/workplace – dampness, irritants?
5. Politicoeconomic:
• Are there constraints on resources that affect breathing, e.g. housing issues, financial issues?
Often assessment is undertaken in difficult circumstances, e.g. emergency admission to hospital is an anxiety-provoking event for patients and their relatives. Crisis intervention within community mental health nursing is another occasion when assessment is required, usually following a series of difficult events leading up to the need for intervention. The initial impression the nurse may have of the patient/client and their family can influence the ease with which the nurse is able to elicit reliable information. If the nurse gives the impression of being disinterested or hurried, it is unlikely that an accurate assessment will be made. Assessment should form the beginning of a trusting relationship between the nurse and patient/client and provides the person with the opportunity of putting their view of their current situation forward. There may be occasions when the patient/client is unable to provide information, through illness, confusion, being too young or having difficulty with communication, e.g. learning disability.
Secondary sources
These are used together with the primary source. Biographical data can be confirmed from previous health records. It is important to confirm the currency of this information in case of changes in circumstances such as someone being widowed or having moved house. Social and medical history can often be confirmed from other health records. Other practitioners can also offer information about patients/clients. For example, key workers of individuals living in residential or nursing homes can provide information if a client is hospitalized. Patient-held records or patient passports are also used, when available. Past medical history is also important to assess along with the current health situation. This can reveal information that may impact on the current situation, such as knowledge of allergic reactions to a drug or relevant information about the person's prior experience. Family members and significant others can also be rich sources of information about the patient/client and how their current situation is affecting their ability to cope with daily living.
Discharge planning
Prevention of early readmission may be avoided if discharge planning is robust enough to support the person on discharge. Inadequate planning and coordination can lead to unnecessary suffering and can also have a major impact on the resources needed to support the person. Preparing a patient/client and their family for discharge from hospital is an integral part of nursing care ( DH 2010c ). In many cases, discharge is the most important aspect of a hospital admission for the patient/client and their family.
As many hospital admissions are very short, planning for discharge should be incorporated into the initial assessment and pre-assessment stage. During surgical pre-assessment visits (see Ch. 24 ), people are given information regarding requirements for going home following surgery or other invasive procedures. If a patient lives alone and is unable to have someone stay with them following discharge after day surgery and/or an anaesthetic, an overnight hospital stay may be more appropriate. Thus social, physical, psychological, economic and environmental aspects of assessment are crucial in providing relevant information that will inform a safe discharge. With many people being discharged following hospital admission for acute problems, or longstanding chronic problems, complex management plans and packages of care may be required and therefore a coordinated approach to discharge planning is necessary. Early supported discharge teams are in place in some specialties such as orthopaedics and care of older adults. Within these services, there is explicit inclusion of discharge criteria in the care planning documentation. The nurse caring for the patient has a responsibility to ensure that a multidisciplinary approach is taken when required. Therefore, discharge planning is documented as an integral part of care delivery, emphasizing the need for the nurse to work in partnership with other professional groups and agencies ( DH 2010c ).
The nature of a patient's health needs or presenting problems will inform discharge planning; for hospitalized patients, nurses also need to enquire about the perspectives of carers. Most patients have a network of significant others who can provide information about them; they must also be consulted about certain aspects of care such as the transition from home to hospital, or hospital to home. Without the support of significant others, it is often not possible to achieve a successful discharge. Patient transfer also necessitates careful planning and communication of all involved. DH (2010c) emphasize the importance of involving patients/clients and carers in the process and to help these principles be applied to transfer situations, a best practice template is available ( Scottish Government 2009 ). Box 14.3 summarizes factors that require consideration before transfer or discharge.
Box 14.3 Factors that are taken into account before a patient is transferred or discharged
• Patient and their relatives are aware of transfer/discharge
• Specific care, e.g. wound care is documented
• Appropriate patient education has been undertaken
• Mode of transport appropriate and organized
• Name of person responsible for transfer/discharge
• Social service involvement needed and organized
• Community services needed, e.g. nurse/multidisciplinary team/home care
• GP letter/immediate discharge document/transfer documentation completed
• Medication ready to go with patient
• Follow-up appointment information available
• Aids/dressings/prosthesis are available
• Access to home has been assessed.
The assessment interview
The planned assessment interview that forms the basis of the nursing history can take place in many settings. The health visitor may conduct an assessment of a child's developmental progress at home surrounded by parents and other family members. Alternatively, the assessment might be in a situation of crisis, such as a serious injury following an accident. Whatever the situation, there must be structure to the interview. The focus will be not only on the documentation being used but also on the person being interviewed. It is important to include both. The use of documentation alone will not allow the whole spectrum of issues to be captured. The first interview allows the nurse to gather baseline information about the person. Comparisons against this will be ongoing. In some settings the interview will be conducted by a doctor and a nurse such as in acute mental health admissions ( Barker 2009 ). The advantage of this is that the client will not have to repeat similar information to different professionals. There is also the benefit of engaging in multiprofessional working, with all health professionals sharing care of the patient to provide a cohesive service ( Barker 2009 ).
At all times during the assessment process, privacy must be respected. This may be easier to achieve in some settings than in others, e.g. when an interview room is available. In the patient's/client's home or in a busy department where there are many other people, it may be more difficult to achieve and therefore careful consideration is needed. In the home it may mean asking other family members to leave the room, or in the department it may be necessary to speak quietly behind screens. Other barriers to effective communication need to be identified and remedied, e.g. environmental noise affecting concentration could be avoided by moving to a quieter area. Language barriers may be overcome by the use of interpreters from within the family or the health provider organization. Confidentiality should be maintained if interpreters are being used. It should be recognized that factors affecting the quality of the interaction between the nurse and the person may have an adverse effect on the quality of information provided and the care received (see Ch. 9 and Box 14.4 ).
Sharing personal information
Before starting your nursing course, you may have had to undergo occupational health screening.
• Reflect on the situation where someone you had not previously met has asked you to reveal personal information.
• Consider how you felt about divulging personal information to a stranger.
• How did the approach of the person affect your feelings at the time?
Interpretation of information
The nurse will undertake a decision-making process to make sense of the data collected from the assessment and formulate a plan of care. Nurses need to be aware of their own beliefs, values and attitudes as well as their level of knowledge and competence. Assumptions should not be made about the condition of a patient/client. Unlike BP measurement, not all patient/client observations, can be validated. For example, it is difficult to measure the level of anxiety a patient is experiencing (see Ch. 11 ). As such, nurses need a degree of self-awareness to ensure that value judgements and assumptions are not made regarding the person's situation.
Staging assessment
The use of a step-wise approach to assessment is sometimes appropriate, with some aspects of the assessment process being undertaken immediately, while others are undertaken later. For example, an older adult being admitted to a care home may have a full assessment undertaken over a period of 1 week to minimize the effects of relocating on their usual routines and ability to adapt. An unconscious child admitted to an emergency department would need immediate assessment to allow priorities of care to be established.
It is sometimes inappropriate to explore every aspect of assessment at the initial interview. In some mental health and learning disability settings, client assessment may be undertaken incrementally as the therapeutic relationship is established. This is also the case in situations when a person is moving into long-term care, e.g. a nursing home. If this is the case, the nurse assessing must take responsibility for ensuring full assessment is completed. This can be useful if the patient/client needs time to adjust to their new situation before discussing sensitive issues with the nurse.
Documentation
Documentation of the nursing process, at each stage, is an important way to communicate to other members of the healthcare team how the patient/client is progressing and responding to interventions. Documentation must be comprehensive and accurately reflect the health status of the patient/client. Accuracy is achieved by recording information precisely, e.g. ‘the patient had 150 mL of tea, and toast and scrambled eggs’ rather than ‘good appetite’, as appetite varies from person to person, and also from nurse to nurse, thus making the assessment subjective. It is a professional requirement to record nursing interventions and the information collected to inform the intervention, as nursing documentation is a legal document ( NMC 2010a ).
Assessment documentation takes different formats according to the setting. Electronic records of care are being implemented gradually throughout the UK as information technology systems are developed to support healthcare delivery ( DH 2010c ; House of Commons 2007 ). Patient-held records are also used, especially for people with long-term conditions. Patient-held records can support self-management and self-care, thus increasing patient involvement. For example, in asthma care when a person attends the practice nurse, the GP and an outpatient department, it is useful for them to have one record that can be used by all professionals to improve continuity of care across primary and secondary care settings. Increasingly, multidisciplinary documentation is being developed with the whole team having access to the records. Confidentiality should be maintained at all times regarding documentation, irrespective of the mechanism being used ( NMC 2010a ).
Single shared assessment is intended to simplify the assessment process, be person-centred and clarify responsibilities between health and social care providers, mainly for older adults in the community. Making this process work, however, requires commitment from all healthcare practitioners to keep the patient/client central to planning of their care. Additionally, this may mean the erosion of traditional professional barriers and boundaries. The underpinning philosophy of shared assessment is that it is ‘needs led’ rather than ‘service led’.
Assessment tools
Assessment tools, as part of risk assessment, form part of the assessment process and those used depend on the specific needs of the patient. Assessment tools, developed by nurses (practitioners and researchers), provide a validated method of eliciting information with a view to minimizing patient/client risk. Tools devised by other professional groups are also used by nurses, e.g. the Glasgow Coma Scale and Paediatric Glasgow Coma Scale (see Ch. 16 ). An example of a commonly used assessment tool is the Waterlow scale, a pressure ulcer risk assessment tool ( Fig. 14.2 ; see also Ch. 25 ). This tool is used to predict the level of risk of an individual developing pressure ulcers, taking their overall condition into account ( Box 14.5 ). Early Warning Score (EWS) charts are assessment tools commonly used to monitor patient's vital signs in order to identify deterioration in condition (see Fig. 14.14 ). Tools should be appropriate to the client group to optimize their effectiveness. Risk assessment (see Ch. 13 ) should be performed at appropriate times, e.g. when there is a change in the health status of a patient/client. It is important that all staff using an assessment tool are familiar with its use.
Using assessment tools
• 2-year-old Jane has been admitted to a children's ward with suspected meningitis. She has a generalized rash and moving is painful
• Isa Oliver (84) has been admitted to an orthopaedic ward through the emergency department after a fall at home. She has previously been in good health and independent at home. She has a fractured hip and is scheduled for surgery today
• Imad Jumaa (68) lives in a nursing home. He has dementia and poor mobility due to arthritis. He is doubly incontinent and is unable to attend to his own hygiene needs. Imad has difficulty with communication
• Fred Maxwell is 28 years old and has a learning disability. He lives in a house with four other service users who are supported by carers. He also has physical disabilities and mobilizes with a wheelchair. Fred is underweight and his appetite is poor; he needs help with personal hygiene and feeding, and is incontinent of urine.
Student activity
Using the Waterlow scale (see Fig. 14.2 ), assess the level of risk the people above may have of developing pressure ulcers (see Ch. 25 for further information, including other pressure ulcer risk assessment tools).
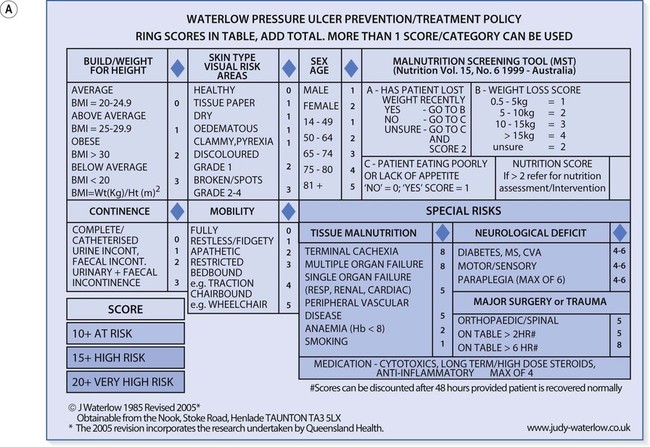
This stage of the nursing process involves identifying the person's problems or needs and what nursing care, intervention or support is required. The care plan should be written down and contain clear statements about how the person's goals will be achieved (see below). The patient/client should also be involved in this stage, if possible. The format of the care plan depends on the particular setting. As well as establishing the person's existing problems, any potential problems are also identified. Learning disability nurses may also concentrate on a client's strengths as well as weaknesses.
Prioritizing care
Planning also incorporates prioritizing care according to the needs of the individual and seriousness of the problems. Life-threatening situations such as airway obstruction must be considered and acted upon before wider health needs, such as the desire to stop smoking. Determining priorities is achieved through an understanding of the theory and concepts underpinning nursing. Involvement of the person in this stage of the nursing process also assists in prioritizing care according to their wishes if there are no life-threatening issues. Through communication, mutually agreed goals can be set, based on the person's perception of their situation.
Actual and potential problems
The aims of planning are to:
• Solve actual problems (or meet health needs)
• Minimize the risk of potential problems
• Reduce recurring problems
• Assist in development of coping strategies for problematical health issues
• Build on strengths.
Consequently, nurses need to be able to ‘see beyond’ the present situation and use their knowledge and expertise to avoid complications and potential problems occurring ( Box 14.6 ). It can be seen from Rashid's situation that the impact of one problem can potentially create many other problems for him that transcend different dimensions of need ( p. 311 ).
Box 14.6 Actual and potential problems
59-year-old Rashid was admitted to hospital with a left-sided weakness and investigations show that he has had a stroke. Rashid is left handed. One of his actual problems is that he is unable to move his left side, which might affect his mobility, skin integrity and independence.
Actual problem
• Unable to move left side.
Potential problems
• Negative impact on self-esteem
• Help required with eating and drinking
• Reduced mobility (see Ch. 18 )
• Pressure ulcers (see Ch. 25 )
• Deep vein thrombosis (see Ch. 24 )
• Muscle weakness
• Limb contractures
• Inability to attend to personal hygiene
• Loss of independence.
Goal setting as part of care planning
Goals are set to enable measurement of the success, or otherwise, of the nursing interventions planned to meet them. Different types of nursing action are often required to meet the goals. For example, different members of the healthcare team may deliver different aspects of the care required. Which member of the team delivers the care to an individual depends on the complexity of their care and on the skills of the members. Competent healthcare assistants may perform some nursing interventions, e.g. they may be able to assist people to maintain personal hygiene. However, for some therapeutic interventions, the registered nurse (RN) would be required to monitor some parameters such as central venous pressure.
Goals can be either short or long term. They should be person centred and achievable. To assist in this, goals should be SMART and incorporate the following characteristics:
• S pecific – state clearly what is to be achieved
• M easurable – be made quantifiable
• A chievable – must be able to be achieved by the patient/client
• R ealistic – possible for the patient/client to achieve
• T imed – have a time limit by which the goal can be achieved and evaluation undertaken.
A goal could be ‘the patient should drink 2.5 L of fluid within the next 24 hours’. Within this goal, it would have been assessed that the patient is capable of taking fluids orally, making it achievable and realistic. It is specific because it states the amount of fluid to be taken, is measurable as fluid intake and is timed as there is a timeframe allocated to its achievement. Box 14.7 provides an example of short- and long-term goals. If goals are unrealistic and unachievable, this can lead to disappointment of both the patient/client and the nurse. As a consequence, the therapeutic relationship may be adversely affected.
Box 14.7 Short- and long-term goals
Eddie has been admitted to the ward with breathlessness. In relation to this, the following goals may be appropriate.
A short-term goal may be:
• To reduce Eddie's respiratory rate to <20 breaths/min within 2 hours
The goal may be achieved by:
• Careful positioning in bed; sitting upright, well supported with pillows or leaning on a bed table (see Ch. 17 )
• Administration of prescribed medication (see Ch. 22 )
• Administration of prescribed oxygen therapy (see Ch. 17 ).
A long-term goal may be:
• To cope with mild breathlessness prior to discharge
• Education regarding breathing exercises prior to discharge
• Teaching Eddie to reduce activity that provokes breathlessness
• Referral to the physiotherapist.
Implementation
Putting the care plan into action forms the implementation stage of the nursing process. Implementation should incorporate current evidence-based practice ( Ch. 5 ). The care plan may encompass physical, psychological, social, emotional and environmental interventions. Implementation may also include activities that are outwith nurses' expertise, e.g. it may be appropriate to refer the patient/client to another healthcare professional such as an occupational therapist for assessment of dressing ability. This referral is the nurse's responsibility and is recorded in the care plan. Such multidisciplinary working and collaboration should assist in providing holistic care.
Evaluation determines if the planned intervention has been effective in achieving the goals set. The goals are reviewed to determine whether or not the patient has met them or is moving towards meeting them. At this stage, the goals can be modified or changed according to the patient's/client's response to the interventions. If a goal has been achieved, this is documented. If a goal has not been achieved, the nurse should question why this is the case, and reassess the patient. Perhaps the goals did not encompass the SMART characteristics or the patient's/client's condition may have changed, making the goals unrealistic. Health needs are dynamic and thus require periodic reassessment. Evaluation is an ongoing action that forms part of the cyclical nursing process. However, evaluation is only possible if clear criteria have been applied to the goals. Evaluation of care can be used as part of nursing audit.
Nursing models
A nursing model, also known as a ‘conceptual model’, is a tool used to guide nurses as they engage in the nursing process and can be viewed as a practical way of putting the nursing process into action. Central to the use of any nursing model is the need for nurses to have excellent communication skills (see Ch. 9 ). There are many different nursing models that reflect the diversity of each field of nursing. Therefore nursing models have different philosophical assumptions underpinning them, each with a unique perspective of nursing knowledge and nursing practice and several are explored in the following sections. Most nursing models are based upon four concepts, which are said to form the essential structure of nursing. The relationship that emerges between the nurse and patient/client will depend on these four concepts:
• The person – the nature of the patient/client having a dimension of ‘wholeness’ or holism
• Nursing – a helping process with interpersonal relationships at its core
• Health – the goal of nursing is to assist people to achieve an optimum state of health, whether or not they are ‘ill’ (see Ch. 1 )
• The environment – the physical constructions of the world and society within it.
Approaches to care planning for adults
Two commonly used nursing models are discussed in this section.

The Roper, Logan and Tierney model for nursing
The Activities of Living model was developed in the UK by Roper, Logan and Tierney who first published the Elements of Nursing in 1980. Their work developed some of the central components of Virginia Henderson's earlier definition of nursing (see Ch. 2 ). There are two parts to this model: the model of living and the model for nursing ( Fig. 14.3 ). Over the years it has been refined, indicating that nursing is a dynamic profession, constantly developing in response to external influences.
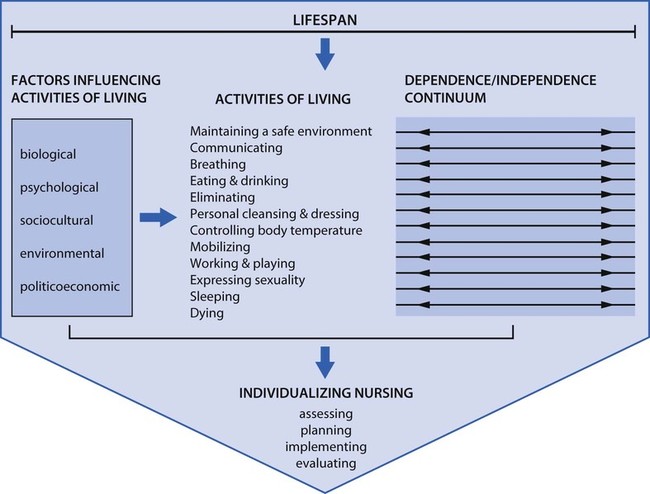
According to Roper et al (2000) , five interrelated components form the core of the model of living:
• The individual
• Activities of living (ALs)
• Lifespan
• Dependence/independence
• Factors influencing the ALs.
The individual
According to Roper et al (2000) , individuality in living acknowledges that each person has a unique way of performing the ALs according to where they are on the lifespan, the degree of dependence/independence they have and the influences of biological, psychological, sociocultural, environmental and politicoeconomic factors. Individuality in living is concerned with how an individual experiences and performs ALs according to their preferences, abilities and attitudes.
Activities of living
Roper et al (2000) suggested that 12 activities are essential for survival:
• Maintaining a safe environment ( Ch. 13 + others)
• Communicating ( Ch. 9 )
• Breathing ( Ch. 17 )
• Eating and drinking ( Ch. 20 )
• Eliminating ( Chs 20 , 21 )
• Personal cleansing and dressing ( Ch. 16 )
• Controlling body temperature (see p. 319 )
• Mobilizing ( Ch. 18 )
• Working and playing ( Ch. 8 + others)
• Expressing sexuality ( Ch. 8 + others)
• Sleeping ( Ch. 10 )
• Dying ( Ch. 12 ).
It is evident that the activities cannot be viewed as mutually exclusive as they are dimensions that interlink with each other ( Box 14.8 ). For example, it is not possible to consider elimination without considering eating and drinking.
The relationship between factors influencing activities of living (ALs) and the interdependence of ALs
Jane is 17 years old and lives with her mother and 11-year-old sister. Jane's parents are divorced and her father is not in contact with them. Her mother has chronic arthritis and is physically dependent on Jane to support her with running the house. Jane helps her mother to get into the shower in the evenings and collects her prescriptions. She also does the shopping, cleaning, ironing and supervises her younger sister with homework and getting ready for school. Jane is at college full-time and on Friday evenings, her friends often go the student union then on to a nightclub. Jane is usually too tired to join them.
• Think about how Jane may experience social isolation from her peers (working and playing).
• Consider the psychological impact that home circumstances may have on Jane (sleeping).
• Identify ways in which Jane could get additional support to ease her situation (maintaining a safe environment).
The lifespan is considered to be a continuum with changes occurring along it from birth to death. Throughout this time, every aspect of living is influenced by biological, psychological, sociocultural, environmental and politicoeconomic factors. The five stages of life identified by Roper et al (2000) are:
• Infancy
• Childhood
• Adolescence
• Adulthood
• Old age.
Throughout these periods, levels of dependence and independence vary. An infant is vulnerable and dependent on others for survival and love. Childhood and adolescence are affected by cultural issues, sociocultural norms and subcultures (see Ch. 8 ) and are dominated by the family. In adulthood, work and family affect lifestyle. In old age, individuals may have an illness that affects their level of independence, e.g. arthritis which can impair mobility.
Factors influencing the ALs
There are five main factors that can influence daily living ( Roper et al 2000 ), as outlined below.
Biological factors
In the context of the model of living, biological factors relate to physical and physiological performance. While there are predetermined genetic influences affecting physical characteristics such as skin colour, hair colour, height or genetically determined diseases such as haemophilia, other factors can also affect physical characteristics and function. In wartime, if a child is deprived of food, growth may be affected, resulting in slower rates of growth and development. Thus, environmental and politicoeconomic issues may also affect physical factors. Biological factors associated with ageing may affect a person's ability to work, thereby impacting on their sociocultural status.
Psychological factors
Mental and intellectual activity begins in childhood and continues through adolescence, adulthood and into older age. The stimuli within these lifespan phases vary. In childhood, development begins through sensory stimuli that can be influenced by family issues such as having siblings who may spend time playing with the toddler. In adolescence, development can be affected by the place of the child in the family and the expectations placed upon them. Thus environmental factors may also influence psychological development. Development across the lifespan is discussed in Chapter 8 .
Sociocultural factors
Ideas, values, knowledge and beliefs are embedded within cultural norms of groups within society (see Ch. 8 ). Thus, many variations exist among the population from which patients and clients will come. Culture is unique to groups of people and can affect the behaviour of individuals. It is important to remember that cultural beliefs may have a profound impact on lifestyle and the responses of people who need to access health services. Dietary practices can have an impact on biological factors; for example, vegetarians may have a low iron intake leading to low blood haemoglobin levels and anaemia. Religion may affect how individuals respond to treatment options, e.g. Jehovah's Witnesses may reject blood transfusion as a treatment option compatible with their beliefs. Therefore sociocultural aspects may impact on biological and psychological factors.
Environmental factors
Environmental factors include housing, the atmosphere, noise and sound. Any of these elements can influence the other factors. Atmospheric pollutants such as carbon monoxide can aggravate respiratory conditions such as asthma, thereby having an impact on biological and psychological factors. Noise pollution can cause anxiety that may impact on psychological and biological functioning, e.g. by causing insomnia and anxiety.
Politicoeconomic factors
The economy, law and the state comprise the politicoeconomic factors that impact on individuals. People are governed by fiscal measures such as the need to pay council tax. Local and national economies also affect people and consequently their behaviour. For example, people on low incomes have limited choices on which to spend their money. Asylum seekers who are given vouchers as part of their financial support may have few choices about where they can exchange them. This may lead to lack of choice and being unable to follow dietary customs, thus impacting on biological and psychological factors.
It can be seen that the main themes of the model are inextricably linked and the activities in Box 14.9 highlight this.
Factors influencing activities of living (ALs)
Groups such as asylum seekers, people with a learning disability and those with chronic illness may have limited control over the five factors that influence ALs.
• Think about the impact of the five influencing factors on the three groups of people above. Draw on any experiences you have had in practice, but if you have not encountered such situations, use the information you have read.
• Think of an occasion when one of the five factors that influence ALs has affected your own well-being and how that occasion affected other aspects of your life.
Roy's adaptation model
Sister Callista Roy developed this model in the USA in the 1960s. It has been refined over the years to make it suitable for nursing in the twenty-first century ( Roy & Andrews 1999 ). The basis of Roy's model is that individuals must adapt to a constantly changing environment. The health of the individual is a reflection of that adaptive process. It is a behaviourist model, as it is concerned with the way in which individuals behave in response to changing circumstances. Behaviourism is the study and observation of how individuals behave.
Roy's behaviourist model is based on the following two philosophical assumptions:
• That veritivity (true values and meaning of humankind, the purposefulness of human existence) is the principle of human nature, i.e. individuals exist with a common purpose of humankind
• That humanism is central to the individual, i.e. that human experiences are central to knowing and valuing.
The model is based on the following two scientific assumptions:
• That there are interdependent parts of an individual, working in unity. Control mechanisms are involved in the functioning of the system, and for every stimulus there will be a range of behaviours.
• The capacity and ability of the individual to respond to the stimuli, from both the internal and external environment, relates to the adaptation level.
Within the model, there are three types of stimuli (systems). These are:
• Physiological
• Social.
Roy and Andrews (1999) state that there is an interrelationship between these three systems, with all of them working together to maintain a balance within the individual. For example, if a person is physically unable to drink fluids due to a swallowing problem they may become dehydrated, and thus the internal body environment may be affected. Equally, if someone is trekking across the desert with no water to drink, their social system is affecting their physiological status as they are unable to access fluid to prevent dehydration. Thus the systems are interrelated and interdependent, interacting with each other at all times.
According to Roy, if an individual adapts to these stimuli, it could be said that they are healthy. Most people cope effectively with constant changes to their internal and external environments. During a heat wave, for example, an individual may drink more fluids, slow down their level of activity and increase the ventilation of their home. An individual who is unable to make these changes, such as a toddler, may be considered to have an ineffective response to the stimulus of heat. If the individual has not adapted to the stimulus, then the role of the nurse is to assist the person to adapt to it. Thus, the focus for the nurse is to identify the stimuli to facilitate adaptation in the individual patient/client. Roy acknowledges the individuality of people and so there will be no complete state of balance applicable to everyone. Therefore, the nurse must recognize the needs of individuals.
Roy discusses the adaptation level of individuals as forming an adaptive range. Behavioural responses to stimuli can be effective, adaptive stimuli or maladaptive. The factors that cause problems of maladaptation are called stimuli and there are three types:
• Focal stimuli – the internal or external stimulus immediately affecting the person
• Contextual stimuli – any environmental factors contributing to the focal stimuli
• Residual stimuli – previous experience or attitudes or beliefs ( Roy & Andrews 1999 ) ( Box 14.10 ).
Thinking about Roy's model
The activities below will help you consider how Roy's approach could affect you as a student nurse.
• Imagine you are driving through busy traffic to an appointment with your tutor and you are late. You are approaching traffic lights and they turn red. Think about the effect that focal, contextual and residual stimuli may have on your judgement.
• Your second clinical placement is far from where you live, and the shift patterns there will cause travelling problems. Consider how the focal, contextual and residual stimuli may affect your adaptation to the situation.
• Suggest two behavioural responses to undertaking an assignment. (For example, an adaptive response may be the creation of a mind map to assist your planning, while an ineffective response would be doing nothing.)
Adaptive modes
There are four adaptive modes within Roy's model that serve as a framework for assessment. It is believed that a person's response to stimuli can be observed in these adaptive modes:
• Physiological adaptive mode – physiological balance, i.e. homeostasis
• Self-concept adaptive mode – psychological integrity, moral, spiritual
• Role function mode – social integrity, managing social interaction
• Interdependency mode – emotional and affective (moods or emotions) behaviour.
Roy states that these four modes contribute towards the promotion of adaptive goals leading to integration and wholeness. Nursing intervention would be required if there is a need deficit.
With Roy's model, assessment is advocated using three stages:
• Stage 1 – examine the adaptive modes; identify if coping is adequate
• Stage 2 – detailed assessment; identify focal, contextual and residual stimuli
• Stage 3 – make a nursing diagnosis based on adaptation status; plan the nursing intervention based on the nursing diagnosis.
Planning should identify SMART patient-centred goals (see p. 310 ) that should incorporate the following:
• Ineffective behaviour to be changed: For example, if a patient is pyrexial (see p. 321 ) the goal may be to ‘assist patient to regain normal temperature range by providing cool drinks, administering antipyretic medication and monitoring temperature 4-hourly’.
• Adaptive behaviours to be reinforced: For example, if a patient has stopped smoking since admission to hospital, the goal may be to ‘provide positive reinforcement and assist distraction from smoking through a range of activities such as listening to the radio, reading health education literature and providing access to smoking cessation helpline’.
This involves exploring whether the goals have been met, thus determining if the adaptation response has been achieved effectively or ineffectively. Reassessment occurs at this stage.
Figure 14.4 shows the nursing process as it relates to Roy's adaptation model.
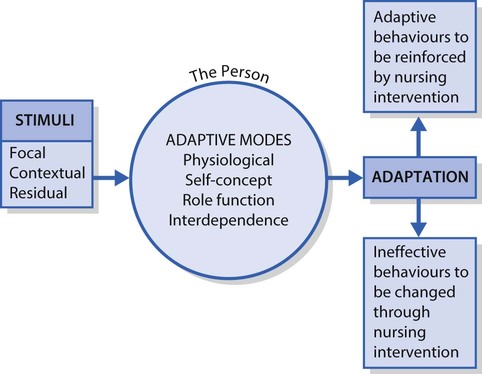
Approaches to planning care for people with learning disability
The focus on the needs of people with learning disability is embedded in national strategies published in the government's White Paper Valuing People ( DH 2001 ). The Scottish Executive (2002) published Promoting Health, Supporting Inclusion, a strategy document to guide practice and the Welsh Assembly Government (2002) has an equivalent, Inclusion, Partnership and Innovation. These strategies, along with societal changes, have provided frameworks for the move towards social inclusion for those with learning disability. The underlying key principles of these documents are:
• Rights
• Independence
• Choice
• Inclusion.
Therefore, in order to care for people with learning disability, these key principles need to be included in the planning process. Individuals with learning disability often have complex health needs. While specialist learning disability nurses are in a strong position to begin to assess and meet these needs, generalist nurses may also assess the person's needs if the four key principles above are encompassed in their care.
When planning care for individuals with learning disability, traditional ways of care planning may not always fully encompass these key principles. Many learning disability nurses consider that nursing models are too focused on the medical model. It is important to use an assessment process that fully involves the person.
It is desirable for people with learning disability to achieve citizenship within the communities in which they live. In order to facilitate citizenship, nurses in all settings need to be able to assist people with learning disabilities to make informed decisions about their health and health issues.
As the spectrum of learning disability is very wide, ranging from mild to profound and complex, the only way to plan and provide supportive care is by placing the individual at the centre of the planning process.
Person-centred planning
Person-centred planning is a way of working in partnership with people and their families to achieve personal autonomy, which is pivotal to realizing the policy aims for people with learning disability ( Scottish Executive 2004 ). As people with learning disability often have unmet health needs, another aim in caring for these people is to help the person have more control over their health ( Scarborough & Godsell 2011 ). For people who have difficulty in articulating their views, an advocate may assist in eliciting their views and thoughts. An advocate may be a paid care-worker or a family member or friend.
Person-centred planning aims to assist people to choose the lifestyle they want. Acknowledgement of the person's disability is made, with acceptance of their need for support on their own terms. The focus is on capacity and capacity building, which means working towards maximizing ability.
Person-centred planning can be achieved by sharing of power between the person, family and professional. Any significant person involved with the client may be involved, e.g. paid support workers or those who act as advocates for the person such as family members. Support workers may be part of the MDT such as learning disability nurses, resource workers, physiotherapists, speech and language therapists, occupational therapists and psychologists. Learning about the person is crucial to developing an understanding of their needs. Careful listening (see Ch. 9 ) and consultation are essential to fully assess the individual. Person-centred planning is a process that takes time and usually starts with a planning meeting. The key features of person-centred planning are shown in Box 14.11 and some are described in more detail below.
• The person is at the centre of the planning process
• Family members and friends are partners in planning
• The plan reflects what is important to the person, the capacities of the person and the support that is required
• The plan leads to actions that are about life, reflecting what is possible and not just about services that are available
• The plan results in ongoing listening, learning about the person and further action (see Sanderson 2007 ).
• Reflect on the extent of person-centred planning you have seen used with people with a learning disability
• Discuss this with your mentor.
Sanderson, H. Person centred planning. In Gates B, ed.: Learning disabilities: Toward inclusion , fifth ed, Edinburgh: Churchill Livingstone, 2007.
Consulting the person throughout the planning process
If the person with learning disabilities has been involved with planning before, it is sensible to talk to them about how they would like to plan, e.g. whether they want a meeting and, if so, what kind of meeting and how they want to be involved. If they are new to planning, it is important to spend time explaining the purpose of planning and looking at different options. Box 14.12 summarizes how this process may work for an individual.
Craig's story
Craig, who is 32 years old, lives at home assisted by his family and a group of part-time support workers. He has learning disabilities, is unable to speak and moves his hands and eyes to communicate. Craig attends a day centre three times a week. While at the day centre, Craig sleeps a lot. His family and support workers describe him as witty and lively, but staff at the day centre find him disinterested and uncommunicative.
It was decided to make a plan for the future. Craig's family asked him who he would like to be involved in the planning. Craig invited staff from the day centre. He asked for the two members of staff he felt most comfortable with. They were happy to come, as they thought that Craig might not be getting the most from his time in the day centre. The meeting was held in Craig's home and took up most of an evening.
During the planning meeting, Craig communicated to the group that he was interested in learning to play a musical instrument, finding a girlfriend and making changes that would allow him to make new friends. It was the first time that anyone had realized Craig had these ambitions and no one thought it was impossible to achieve them. Staff from the day centre then recognized that the reason Craig was different at the day centre was probably because he felt he did not know the staff well and they did not know fully how to communicate with him.
The people who attended the meeting then worked together to change things. Craig now attends a weekly music class with a support worker. One of the staff from the day centre has spent time in Craig's home to get a better understanding of his needs. The next stage of the plan is to find other activities that interest Craig and, like the music class, he will attend these with a support worker. In time, it is planned that he will reduce the time he spends at the day centre as other activities increase. Things are slowly changing for the better and Craig is now involved in every decision that is made.
Visit the Scottish Consortium for Learning Disability website ( www.scld.org.uk ) and find out how one agency is trying to achieve the goals of the government strategies for people with learning disability.
The person chooses who to involve
Unlike traditional planning, it is for the person with learning disabilities to decide who they want to include in the planning process and how. This is easy to say but, with existing services, this is very different from the way meetings are typically organized. If the people around those with learning disabilities cannot find a way to help them make and communicate that decision for themselves, then they must decide in good faith who they think the person would want to involve. A good starting point is thinking about ‘people who know and care about the person’, which may well yield a different answer from ‘people who provide a service to this person’.
The person chooses the setting and timing of meetings
If a meeting takes place it should be at a time convenient to the person with learning disabilities, with the people they wish to invite and be in a place where they feel ‘at home’. The planning should be carried out in a way that is accessible to the person with learning disabilities. Graphics, tapes, videos or photos are often used.
Approaches to planning care in mental health nursing
In common with learning disability nursing, mental health nursing has also been driven by policy development to become user focused. The trend towards community-based care continues with many services provided by mental health nurses. There is emphasis on caring for people who have enduring mental illness such as schizophrenia. The shift away from institutional care has led to examination and scrutiny of approaches to planning and implementation of care. The following key principles underpin care planning in mental health settings:
• Advocacy
• Consent
• Autonomy
• Relationships
• Communication
• User involvement.
In mental health nursing, the approach used is also person-centred ( Barker 2009 ). A person-centred approach builds on the seminal work of Peplau (1952) who espoused the strengths of the therapeutic relationship between the nurse and the person. Building on the work of Peplau is the notion of the professional relationships the nurse has with other professionals as well as the need for a person-centred nurse/person relationship that is not driven by the power of the nurse ( Barker 2009 ).
The Tidal model
The Tidal model ( Barker 2009 ) was initially developed from a study into mental health nursing. It is a multidimensional approach to the provision of mental healthcare. The philosophy is that people can recover from the experience of mental health problems and that nurses can assist clients to return to their daily life. Therefore, the philosophy is about helping people to cope with their problems and find solutions through their own experiences. As it is not about ‘fixing them’, this model has an empowering approach.
The Tidal model represents the unique contribution that nurses make to the care of people with mental health problems, though it also acknowledges the close relationships with other health and social care practitioners. One of its features is that a care continuum exists. The care continuum straddles the primary and secondary care settings with the premise that the needs of the person should be the focus of care rather than the setting. The assumption is that the need for nursing lies wherever the person is and not within the ‘compartments’ of primary or secondary care. Other features of the model are:
• Active collaboration with the person and family, if appropriate, to plan and deliver care
• Empowerment of the person through the narrative of illness and health
• Integration of nursing with the services provided by other members of the MDT
• Resolution of problems of living and promotion of mental health through narrative-based interventions in individual and group sessions.
The role of the nurse is two-fold:
• To form a therapeutic relationship with the person and, where appropriate, the family
• To cultivate professional relationships with other workers and professionals who may be involved in the care of the individual.
Barker (1996, p 236) illustrates the core basis of the Tidal model:
Life is a journey undertaken on an ocean of experience. All human development, including the experience of illness and health, involves discoveries made on the journey across that ocean of experience.
At critical points in the life journey the person experiences storms or even piracy (crisis). At other times the ship may begin to take in water and the person may face the prospect of drowning or shipwreck (breakdown). The person may need to be guided to a safe haven to undertake repairs, or to recover from the trauma (rehabilitation). Once the ship is made intact or the person has regained the necessary sea legs, the ship may set sail again, aiming to put the person back on the life course (recovery).
Barker (1996) asserts that there are three dimensions within the model:
• World – the need to be understood, including having the personal meaning of illness and distress validated by others
• Self – emotional and physical security
• Others – medical, psychological and social interventions, e.g. housing, finance, occupation, leisure.
The aim of assessment and planning within the three dimensions is to allow the person to verbalize their own experience to determine how their needs can be met. The narrative basis of the model suggests that the ‘self’ of the person-as-the-expert can be explored through careful inquiry by the nurse. Therefore, the therapeutic relationship between the nurse and person is crucial to allow construction of the person's experience through narratives. The care plan should document the needs of the person expressed in their own words rather than in professional language or in the third person. Thus the lived experience of the person can be documented.
The aim of the Tidal model, using a person-centred approach, dovetails with best practice statements regarding engagement with the person to work towards person-centred care ( Barker 2009 ).
Further information about approaches to mental health nursing can be found in Useful websites, p. 335 .
Approaches to planning care for children
Partnership in care is advocated as the desired approach to caring for children recommended in the National Service Framework ( DH 2003 ). Every Child Matters, the government strategy that followed The Children Act 2004 ( HM Government 2004 ), provides further aspirations and policies about the integrated partnership approach to caring for children across society (see Chs 3 , 6 ). The services that children require change as they develop and encounter illness or vulnerability. The key to providing excellent care is in the relationships that develop between the nurse, the child and the family as well as those that the nurse has with other professional agencies and services. Respecting parents and the family means recognizing that:
• Parents are usually the expert on the child
• Parents may have other children to care for and may need to balance the needs of the other children and the child requiring care
• Parents may have to take time off work to attend outpatient or primary care appointments, or during hospital admission
• Parents may have health issues themselves which may influence their ability to be fully involved with the child
• Healthcare and hospitalization can impose financial hardship on the family ( DH 2003 ).
The Nottingham model ( Smith et al 2002 ) and Casey's partnership model ( Casey 2007 ) are prominent in children's nursing. Both models are based on respect for the wishes of the family and negotiation of care needs. The main differences between them are that the Nottingham model includes the child and the family as ‘the client’, whereas Casey views the child as ‘the client’. However, a partnership approach is central to them both.
The Nottingham model
While the philosophy of this model includes the family members as partners, it is still important to include the child in the decision-making process where possible. By doing this, dignity and respect for the child are maintained. As the model uses a holistic approach, taking account of the wider influences that can affect a child's health, the family's perception of health in relation to the child should be assessed when the history is being taken during admission.
Hospital admission can be very disruptive, not only to the child but also to the wider family. The child may have alteration in normal functioning that spans the physical, psychological, social, emotional and/or environmental dimensions of life ( DH 2003 ). To minimize the trauma associated with hospital admission, a welcoming environment is necessary to enable the process of negotiated care to be established. A routine that allows a child's normal activities to be undertaken in relation to activities of living is encouraged, particularly in respect of education and recreation. Play is an important element of the nursing care provided (see Chs 8 , 9 ) and forms an important aspect of pain management (see Ch. 23 ). The family or main caregivers should be considered the experts on young children. Their knowledge of the child's behaviour and level of independence can be communicated to the nurse and the plan of care is developed jointly. Assisting the family to retain some control over their lives, while meeting the needs of their child, is desirable. This often means that the family will be involved in direct care giving. To provide this type of family-centred care, the family must have clear guidelines about what to expect from the nurse. Therefore, nurses caring for children need to be excellent communicators. Older children and young people are often the experts about their own conditions and associated care.
If hospital admissions are planned (elective), some of the fear associated with hospital admission can be allayed. Receiving written and verbal information prior to admission may help reduce anxiety for the child and their family. It may also reduce recovery times. Preadmission schemes can also reduce some of the fears and anxiety by providing an opportunity to visit the environment and meet with some of the staff ( Smith et al 2002 ). The Nottingham model follows the steps of the nursing process from assessment, planning, implementing and evaluating care.
Negotiated care
Negotiated care refers to a two-way process between the nurse and the child and their family. The relationship between these people should be based on mutual trust and respect. With each person's contribution being equally valued, an agreed plan of care can be made. The process of negotiation begins at the assessment stage. The level of family involvement should be frequently reassessed as the situation may change, as can the needs of the family. Thus parental participation in direct care delivery may vary over time.
Building an equal partnership
An equal partnership can be developed through the nurse assisting the family to acquire the additional knowledge and skills of caring needed. Equipping the family with knowledge can empower them. Factors that can build the partnership include:
• A positive attitude of the nurse that includes the family in care delivery if desired
• Willingness of the nurse to share information, knowledge and skills
• The ability of the nurse to educate, teach and support others.
Casey's model
This also incorporates negotiated care and partnership building with the child and family. According to Casey (2007) , the key elements of paediatric nursing assessment are:
• The nature of the health problem and the child and family's understanding of it
• The developmental effects the health problem has on the child
• The family's situation, its responses to the problem and the nature of the coping
• The wishes of the family and educational needs
• The usual routines of the child
• The child and family's expectations of care and treatment.
Integrated care pathways
As an alternative to nursing care plans, integrated care pathways (ICPs) may be used. ICPs are sometimes called integrated care plans, care protocols or care maps. There has been increasing development of integrated care plans for all groups of people. The focus on providing a high quality service has led to increased use of ICPs as they are based on the current evidence base for best practice. Much of this evidence is informed by the National Institute for Health and Clinical Excellence (NICE) and the Scottish Intercollegiate Guidelines Network (SIGN). The ICP is a single document in which all members of the multidisciplinary team (MDT) record their care. The ICP details expected problems, interventions and outcomes for a specific disorder or group of people. These are devised with explicit agreement by local groups of multidisciplinary and multiagency staff. The aim is to provide a comprehensive service to a group of service users or patients with a specific condition ( National Leadership and Innovation Agency for Healthcare 2005 ).
The MDT agrees on the format of the record that will be used by all professionals, not just one group, e.g. nurses. The pathway anticipates the expected requirements for care and the outcomes for the patient within a specified timeframe. SMART goals (see p. 310 ) are incorporated into the care pathway. It is still important to have the patient at the centre of the care pathway to ensure that the required standard of care is met. Individual assessment is still undertaken, often based on the assessment process associated with a nursing model. It is important that the philosophy of the assessment meets the needs of the patient/client group. For example, a patient undergoing surgery that may impact on their self-image, such as limb amputation, needs to be assessed psychologically and emotionally to determine their ability to adapt. Thus, the assessment may be based on Roy's adaptation model. So, although the ICP is multidisciplinary, within its development it is vital that the nursing approach is robust enough to incorporate holistic care ( Box 14.13 ).
Having a single document can help to provide an integrated approach to care, with shared working between professionals encouraging greater understanding of others' roles and responsibilities.
Find an ICP used in your placement and then consider the following:
• What benefits are there for the relationships within the MDT when ICPs are used?
• How might the nature of the relationships of MDT members impact on the standard and quality of care given to patients/clients?
• What benefit might there be to patients/clients when ICPs are in use?
The benefits of using ICPs include:
• Enabling monitoring of standards of care
• Transparency of documentation
• Enhanced understanding of other professional roles
• Improved team working
• Explicit goal statements.
There are often reasons why a patient will not follow the expected path of recovery or response such as the presence of other health issues from any aspect of their life, i.e. physical, psychological, emotional, spiritual, sociocultural or environmental. This does not necessarily mean that the pathway is unsuitable for the patient, but rather it may highlight the unique features of any individual who requires care. If a patient varies from the expected pathway, this is documented on the care pathway, including whether the variance was avoidable or not. For example, other diseases impacting on patient progress is unavoidable whereas a delay in having a test performed is avoidable.
Documentation and record-keeping
Documentation and record-keeping apply to every aspect of nursing intervention. Accurate record-keeping is an essential and integral part of professional practice and personal professional development ( NMC 2010a ; see also Ch. 7 ). Records may be required for legal purposes (see Ch. 6 ) and audit. The quality and accuracy of record-keeping can reflect standards of care.
Timely and accurate records may highlight changes in a patient's/client's condition by providing a graphical record of their health status, demonstrating trends and changes over time, e.g. with charts used for baseline observations (see Fig. 14.14 ). Clinical observation charts are used to record vital signs and to calculate an Early Warning Score (EWS, see p. 332 ) which is used to monitor acutely ill patients for signs of deterioration ( NICE 2007 ).
Vital signs
Assessment of a person's health status includes the measurement of vital signs that include temperature, blood pressure, pulse and respiratory rate. These are measures of a person's airway, breathing and circulatory function. In hospital settings, the observations will be recorded on an observations and Early Warning Score chart.
It is of fundamental importance that nurses can competently measure and record the vital signs and respond to change appropriately. The process of measuring, recording and interpreting vital signs demands accuracy. The NMC (2010b) requires student nurses, before the end of progression point 2 (usually at the end of Year 2), to be able to accurately measure and record vital signs and respond to any findings outside the normal range. A further NMC (2010b) requirement is that ‘a baseline assessment of height, weight, temperature, pulse, respiration and blood pressure are accurately undertaken using manual and electronic devices’.
This section uses an evidence-based approach to measuring vital signs. A number of factors can influence the information obtained from these measurements, including changes to the environmental temperature or metabolic activity and exercise or eating. Nursing care of people with abnormally high and low body temperature is explained. At the end of this section, measurement of height and weight is described. These measurements indicate general health or underlying illness that may require investigation, monitoring and/or treatment.
Nurses measure, record and interpret vital signs and use the information to plan and implement appropriate nursing interventions as well as to evaluate the effect of care and treatment. Vital signs are usually all measured at the same time.
Body temperature
Core body temperature in health is in the range of 36.4–37.3° ± 0.2°C. It is measured in degrees (°) Celsius (C), and is relatively constant. Body temperature is an indicator of the balance between the amount of heat being generated by cellular processes and the excess that is lost. Efficient cellular metabolism requires the maintenance of body core temperature and organs that are located within the core, such as the brain, heart and liver, function best around 37°C. This is called the ‘set point’ and serious problems occur if temperature deviates much from this.
Distribution of body heat
Heat is generated by cellular metabolism; therefore areas of high metabolic activity such as the liver or exercising skeletal muscle have the highest temperatures. The locations that best reflect the body's inner or ‘core’ temperature are the heart and brain. Peripheral regions, which are nearer to the environment, are cooler as they are more exposed to the lower ambient temperature outside the body. Temperature sensors placed on the skin surface estimate peripheral or ‘shell’ body temperature. Body core temperature (BCT) can be measured using instruments that may be placed in sites such as the ear canal, oral cavity, axilla or rectum. Figure 14.5 shows body temperature at different sites.
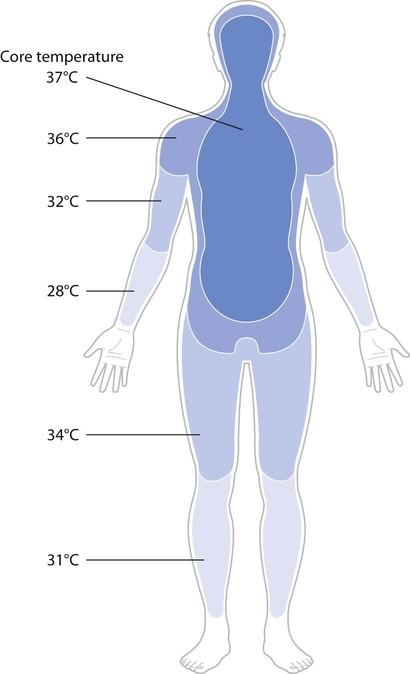
Heat balance
Maintaining body temperature within the normal range requires a balance between heat produced by the body and its loss to the environment. Heat balance is achieved through the interplay of mechanisms that conserve heat and others that promote heat loss.
Heat conservation
When sensors in the hypothalamus detect a fall in temperature they trigger responses that promote heat conservation. These include:
• Vasoconstriction – peripheral blood vessels constrict, diverting blood away from the extremities, thus limiting heat loss from the body to the environment
• Piloerection – body hairs are erected, trapping warm air against the body surface (skin)
• Shivering – generates heat
• Reduced sweating – facilitates heat conservation.
Behavioural responses include putting on more clothes, exercising or moving towards a source of heat.
If core temperature rises above the set point, the body initiates physiological mechanisms that promote heat transfer. These include:
• Vasodilatation – dilatation of peripheral blood vessels, which facilitates heat transfer to the cooler environment of the skin
• Increased sweating – facilitates heat loss as sweat evaporates from the skin
• Increased rate and depth of respirations – promotes heat loss in expired air
• Decrease in cellular metabolism – reduces heat production.
Behavioural mechanisms activated by the brain also promote heat loss. These include taking off clothes or wearing lighter clothes, drinking cold fluids or lifting the arms away from the body.
Physiological influences on body core temperature
There are several factors that influence BCT, as outlined below.
Diurnal cycles
BCT varies throughout the day. Variations are normally within a range of 0.5–1.0°C over 24 hours, with the highest point of 37.2°C at around 18 : 00 hours and lowest (36.7°C) around 06:00 hours. People having their temperature measured daily should therefore have this carried out at the same time each day to avoid normal diurnal variations.
In infants, temperature regulation is labile because their physiological heat-regulating mechanisms are immature, and this can continue until puberty. Babies and small children therefore need to be dressed appropriately for the environmental temperatures around them. Heat production is increased in infants and children due to deposits of brown fat around the neck, back and viscera (the organs within the abdominal cavity). The only role of brown fat is to generate heat, and therefore shivering is not usually observed in this age group. Children also have a higher basal metabolic rate than adults, due to increased tissue growth rates. The consequence of a higher metabolic rate is a higher mean BCT.
Older adults may have a lower mean BCT that is also more influenced by ambient temperature. Therefore, should an older person develop an infection, BCT may not rise significantly. Ageing processes tend to reduce muscle mass, which reduces heat production capability in older adults. Additionally, loss of subcutaneous tissue (insulating fat) and reduced basal metabolic rate influence heat loss and production.
Menstrual cycle
Hormones released throughout the menstrual cycle also influence temperature. Increased cellular metabolism occurs at ovulation and body temperature rises by up to 1°C for the remainder of the cycle.
Other factors
Exercise increases heat production. Stress, pain and illness can also increase body temperature, whereas fatigue and headache can decrease it.
Environmental influences on body temperature
Environmental temperature extremes can raise or lower body temperature. The changes depend on the extent of exposure, air humidity and the presence of convection currents. Smoking cigarettes or cigars can increase oral temperature.
Care of people with temperature abnormalities
Body temperature can deviate from the normal range as a result of excess heat production, minimal heat loss or minimal heat production. It may:
• Rise resulting in pyrexia (fever, BCT above 37.5°C) or hyperthermia (BCT above 40°C) due to failure of heat loss mechanisms (see Further reading , Childs 2011 )
• Fall, resulting in hypothermia (BCT below 35°C).
Disorders such as heatstroke, hypothermia and frostbite may occur when environmental temperatures are extreme. The first aid for people with heatstroke is outlined in this section.
Caring for patients with pyrexia or hyperpyrexia
Pyrexia is present when elevated temperature readings have been recorded at different times throughout the day, rather than a single raised reading. Pyrexia is often caused by an infection and has three stages. The first stage, during which BCT rises, can induce vigorous shivering or ‘rigors’. Shivering generates metabolic heat with a subsequent rise in BCT, which the body uses to mount a response against the invading pathogen. The stages and the nursing care required are outlined in Table 14.1 . Elevated BCT increases basal metabolic rate and oxygen consumption and, in hyperpyrexia, there is serious disruption of brain and other organ function. Children under the age of 5 years are prone to febrile seizures and the first aid needed is described Box 16.32 ( p. 391 ).
Pyrexia: phases and nursing interventions
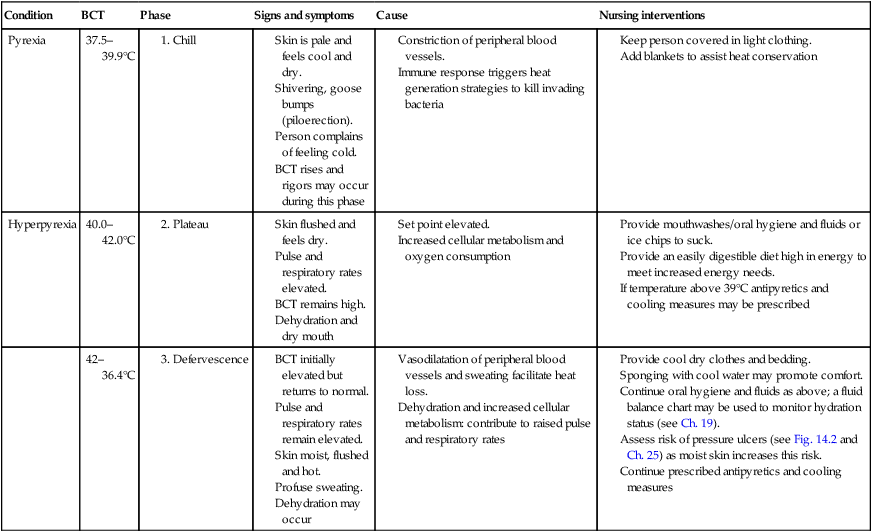
Two major strategies can be used to manage elevated body temperature:
• Antipyretic medication, e.g. paracetamol, ibuprofen, aspirin (not used for children under the age of 16 years because of the potential risk of Reye syndrome, see Ch. 23 ) that reduce BCT
• Cooling interventions. The rationales to support cooling strategies are presented in Table 14.2 . However, cooling patients remains an area of nursing practice that is ritualistic and lacking in conclusive evidence.
Advantages and disadvantages of cooling interventions
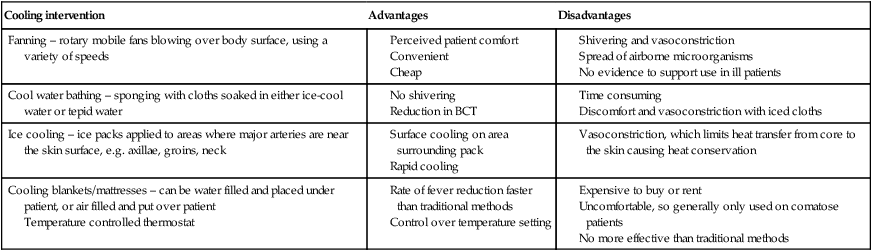
Aggressive forms of cooling such as the use of cooling mattresses or covering the whole body with ice are sometimes required for patients who develop temperatures above 41°C as this may cause serious and sometimes fatal consequences.
Prolonged exposure to hot sunlight or high environmental temperatures can result in the development of a serious condition known as heatstroke where measured BCT can be as high as 45°C. People at risk include:
• Those exercising or engaging in strenuous activity in high environmental temperatures, especially when combined with high humidity
• Children
• Older adults
• Those with co-existing heart disease or metabolic disturbances, e.g. diabetes or hypothyroidism
• Those taking recreational drugs such as Ecstasy, alcohol or medications such as diuretics (see Ch. 22 ) that may impair heat loss mechanisms.
Recognition of heatstroke and the necessary interventions are shown in Box 14.14 .
Recognition
Usually there is sudden onset of some or all of the following signs and symptoms:
• Hot dry skin
• Flushed skin
• Headache
• Excessive thirst
• Nausea
• Numbness, tingling, muscle cramps
• Dizziness
• Restlessness
• Mental confusion.
Observations
• Temperature above 40°C
• Tachypnoea (increased respiratory rate)
• Tachycardia (pulse rate >100 b.p.m. in an adult).
Aims of treatment
• To recognize the presence of heatstroke
• To remove the cause
• To reduce body temperature
• To transfer the casualty to hospital.
• Remove the source of heat – move casualty into shade or out of the sun
• Lie casualty down and provide reassurance
• Loosen clothing and remove any items of unnecessary clothing if possible
• Sponge with cool water
• Dial 999 (or 112) for an ambulance
• Check and record respiratory rate, pulse rate and level of response.
Caring for patients with hypothermia
Hypothermia is present when BCT is below 35°C. It is described as mild, moderate, severe or profound and can be fatal if untreated. Hypothermia usually occurs accidentally as a result of exposure to low environmental temperatures and people at the extremes of age are the most vulnerable. Awareness of and providing interventions that will minimize the risk factors for hypothermia can often prevent its occurrence. Risk factors in infants, adults and older adults are outlined in Box 14.15 .
Box 14.15 Risk factors for hypothermia
• A large surface area in relation to body weight. As the skin is a heat exchanger, heat loss is relatively high
• Their inability to put on more clothes or turn the heating up when feeling cold.
• Cold environmental conditions such as when hillwalking or skiing, especially when not wearing appropriate clothing, and water sports accidents, which result in immersion in cold water that leads to very rapid heat loss
• Excessive alcohol consumption and drug misuse both cause vasodilatation and impair perception of the cold. As a result, people may become inadvertently exposed for prolonged periods.
Older adults
• Impaired ability to control body temperature
• A reduction in temperature sensor (thermoreceptor) effectiveness
• Poor nutrition due to loss of appetite or physical constraints that make it difficult to cook; a low dietary energy intake will reduce heat production
• Loss of the shivering reflex
• Environmental factors such as living in a cold house with little money for heating.
Hypothermia can also occur in hospital. For example, some anaesthetic drugs lower BCT, as do some interventions, e.g. infusing large volumes of unwarmed fluids or irrigating body cavities with cool fluids in theatre. It is therefore important that temperature is carefully assessed and monitored postoperatively (see Ch. 24 ).
Restoring low BCT to normal requires careful management. The following parameters should be assessed: blood pressure (see p. 327 ); heart rate (see p. 325 ); respirations (see p. 330 ); oxygen saturation (see Ch. 17 ); temperature (which should be measured using a tympanic thermometer, see p. 323 , or an internal probe) and urine output.
Management involves warming, which can be active or passive depending on the severity of hypothermia; however, it is dangerous to rewarm a patient too quickly. In mild hypothermia, the aim is to increase BCT by 1–2°C per hour and this can be achieved by: closing windows and doors; leaving clothing on if the room is cold, but taking off any wet clothes and wrapping the person in blankets. Other strategies include: wearing a hat to minimize heat loss through the hea d; particularly for babies and young children, blowing warm air over the body and warming intravenous fluids in moderate and severe hypothermia.
Body temperature assessment tools
Estimation of body core or peripheral temperature can be made at different sites using a variety of instruments, which include tympanic membrane probes, electronic thermometers and disposable chemical dot thermometers.
Each device has advantages and limitations (see Table 14.3 ) and therefore individual needs must be assessed. Should intervention to manage abnormal body temperature be required, it is necessary to select a thermometer that can be used to make frequent or continuous measurements. This must be accurate and reliable at the top and bottom of the scale, and be appropriate for the person's age and individual needs.
Sites and thermometers – a comparison
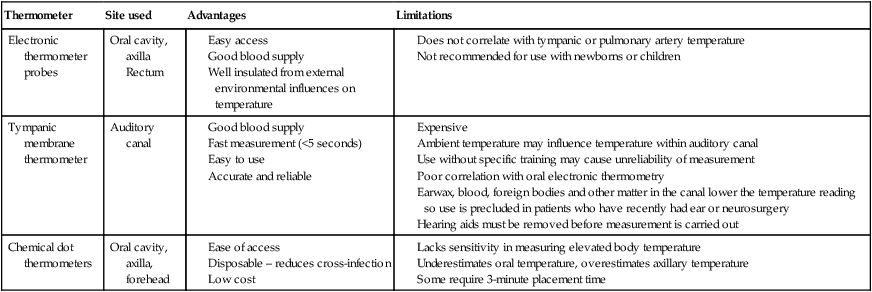
Electronic thermometers
The electronic thermometer ( Fig. 14.6 ) is a battery-operated device that displays a digital readout of the temperature measured during a preset recording time, usually between 20 and 50 seconds. Attached to the device by a cable is a probe, which is most commonly placed in the mouth, axilla or rectum. Protecting rigid probes with a plastic disposable cover and cleaning them between each use prevents cross-infection.
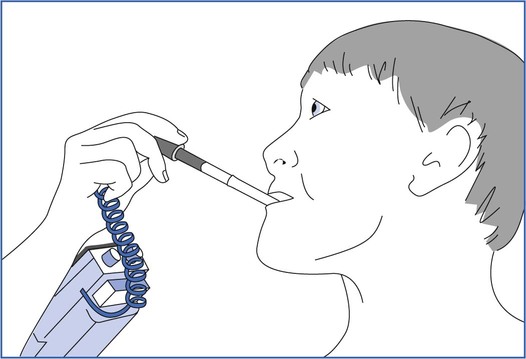
However, the device requires regular calibration, and the site used to measure temperature influences reliability. For example, the axillary placement is affected by environmental temperature and the oral placement depends on its position within the mouth and the cooperation of the patient.
Tympanic thermometers
Tympanic thermometers measure temperature at the tympanic membrane (eardrum). Because the tympanic membrane is in close proximity to the hypothalamus, measurement here accurately reflects the BCT. The tip of the instrument contains a probe, protected by a disposable sheath, which is placed into the ear. Some manufacturers recommend that the pinna is pulled upward and back for an adult and down and back for a child. This action straightens the external ear canal, creates a seal from external air temperature and facilitates correct insertion of the probe ( Fig. 14.7 ).
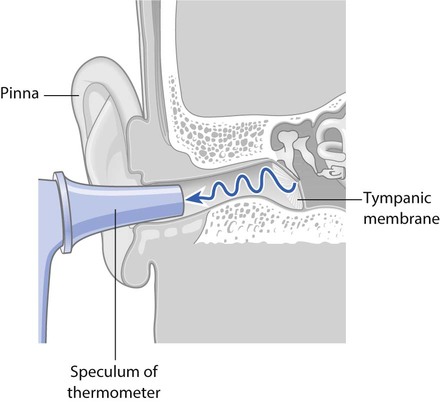
The probe detects heat emitted from the tympanic membrane in the form of infrared energy. The resulting signal is processed and displayed as a digital readout. Temperature is measured and displayed within 3 seconds of activation and the instrument bleeps on completion. The tympanic thermometer measures body temperature accurately between 25° and 43°C.
Tympanic thermometers are widely used in healthcare settings, because they are convenient, easy and quick to use, and reliable. Their limitations are summarized in Table 14.3 .
Single-use thermometers
Single-use thermometers, such as chemical dots, are convenient, easy to use, non-invasive and also disposable. The thermometer consists of a plastic strip, with a series of chemically impregnated paper dots, which is placed in the oral cavity or the axilla. The dots change colour with heat. The final reading can usually be taken in up to 3 minutes, depending on the manufacturer's instructions. Their limitations are summarized in Table 14.3 .
Glass-and-mercury thermometers
These were used for many years, however risks to health from mercury toxicity and dealing with spillages in healthcare settings means these are now seldom used in healthcare settings.
Thermometer placement sites
Temperature varies widely throughout the body (see Fig. 14.5 , p. 320 ) and it is therefore important to remember that, if a temperature trend is required, the same site is used for each measurement. As a result of site variation of temperature, it is erroneous to believe that one location is more accurate than another. For example, BCT measured at the pulmonary artery is usually higher than the oral or axillary sites because the mouth and skin are exposed to the cooling influences of ambient temperature. In contrast, BCT will be lower than that found in the rectum due to the heat generated from metabolic activity of microorganisms in the rectum. Commonly used sites for measuring body temperature include the oral cavity, the tympanic membrane, the axilla and the rectum, which are discussed below. Measurement of blood temperature within the pulmonary artery is considered to be the most accurate reflection of BCT – the ‘gold standard’. This is because blood returning from major organs to the heart reflects the average temperature of the major internal organs. However, measuring pulmonary artery blood temperature is an invasive technique that is confined to critical care areas as are other sites including the pharynx, oesophagus and bladder.
Oral cavity
The thermometer is placed in the sublingual pocket at the junction with the tongue, which is close to the sublingual artery and therefore equates well with BCT. This site may not be suitable for young children who are at risk from biting the probe, especially if they are afraid and/or uncooperative.
Tympanic membrane
The probe is placed in the auditory canal and can be used for adults or children ( Fig. 14.7 ).
An electronic or chemical dot thermometer is placed under the axilla and the arm holds it in place. This site can be used for adults, infants and children. In children, the arm is held gently against the body to keep the thermometer in place.
The rectum can be used for adults, although it is not commonly used in children in the UK. It is never used in newborns because of the risk of rectal perforation. If a non-disposable temperature probe is used, a disposable sheath is applied and discarded after use. The thermometer is cleaned according to local policy before and after use.
A disposable probe attached to the skin surface can be used for adults or children.
Interpreting temperature measurements
The temperature measured should be recorded. In hospitals, this is usually on a clinical observation chart (see Fig. 14.14 ). Measuring and recording the temperature onto the chart, either every few hours (1–4 hourly) or daily, will reveal a trend for body temperature. If body temperature is elevated above the normal range, then cooling interventions can be initiated (see p. 321 ). Recording the body temperature every few hours while a patient is being cooled will demonstrate whether the strategy is lowering the temperature effectively. The temperature reading should be entered on the clinical observation chart and also contributes to the Early Warning Score (see Fig. 14.14 , p. 333 ).
Nurses frequently perform assessment of the pulse, which is the rhythmic expansion and relaxation of an artery caused by ejection of blood from the left ventricle when it contracts. Knowledge of the rate, volume and rhythm produces information that assists in assessment and evaluation of health status or response to interventions. This section outlines anatomy and physiology of the pulse and explains how it is assessed.
Principal pulse points
The pressure wave, or ‘pulse’, of blood travelling along some arteries can be felt using the fingers at points of the body, where an artery lies close to a bone ( Fig. 14.8 ). This is the ‘peripheral’ pulse, and it can be assessed by palpation (gentle compression of an artery using the fingers, against a bone). The most commonly used site is the radial artery at the wrist ( Fig. 14.9 ).
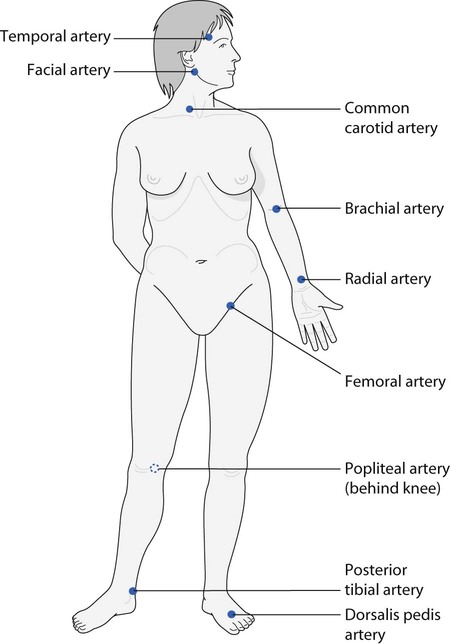
The carotid arteries are located in the neck at each side of the larynx (see Fig. 14.8 ). They supply blood to the brain and are easily accessible. This is sometimes referred to as a central pulse. However, only light pressure should be applied to one artery at a time, in case the blood supply to the brain is restricted. During cardiopulmonary resuscitation, the carotid artery is palpated by trained healthcare practitioners to detect the return of a pulse (see Ch. 17 ).
The femoral artery may be used to assess the pulse, especially when the blood pressure is low as peripheral pulses in the arm and lower leg can be difficult to palpate. Peripheral vascular disease restricts blood flow to the lower limbs and it may be necessary to establish the presence of pulses in the legs to confirm blood flow to the extremities. The popliteal, posterior tibial and dorsalis pedis (also known as ‘pedal’) pulse sites are used to assess whether circulation is present in specific parts of the leg and foot. The popliteal pulse can be difficult to palpate and considerable practice may be required to master this.
Normal pulse rate
The rhythmic pulsation of blood in the arterial system is counted and recorded as the pulse rate ( Box 14.16 ) and normally represents the rate at which the heart beats, i.e. the heart rate. The normal resting rate in adults is between 60 and 100 beats per minute (b.p.m.). In adults, tachycardia is the term given to pulse rates greater than 100 b.p.m.; bradycardia describes a pulse rate below 60 b.p.m.
Taking the pulse
• Watch with second hand
• Observation chart.
Preparation
• Explain the procedure and seek verbal consent; maintain respect and dignity at all times
• The person should be lying or sitting down. Allow the person to rest for 30 minutes after physical activity, emotional upset or smoking
• Wash hands as per local policy.
• Select the pulse site
• Apply pressure gently but firmly with flat fingers until the pulse is palpated
• Count the number of beats for 1 minute using a watch with a second hand. If a regular rhythm is noted, the pulse can be counted for 30 seconds and the number of beats is doubled
• Note further characteristics of the pulse:
• rhythm (regular or irregular)
• force or volume
• If the respiratory rate is to be measured, this is usually carried out discreetly while recording the pulse (see Fig. 14.13 )
• Wash hands according to local policy
• Record pulse rate on the observation chart (see Fig. 14.14 )
• Report and document any changes/abnormalities.
This important skill forms part of Essential Skills Cluster 9 ( NMC 2010b ).
Factors that affect heart rate
The pulse rate varies depending on the degree of activity within the autonomic nervous system. Stimulation of the sympathetic nervous system and the release of adrenaline increase heart rate, whereas parasympathetic activity decreases it. Due to their higher metabolic rate, children have a faster pulse rate than adults (see Table 14.4 ).
Pulse rates for children
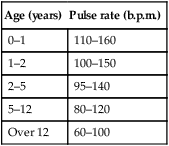
(Reproduced with permission from Mackway-Jones, K., Molyneux, E., Phillips, B., et al. (Eds.), 2005. Paediatric life support: the practical approach, fourth ed. BMJ Books/Blackwell, Oxford.)
Stressors such as pain, fear and anger increase the pulse rate as they increase sympathetic activity. The rate also increases with exercise and pyrexia, and may alter due to the effects of medications and some diseases such as those involving the heart, lungs or blood (see Ch. 17 ). Medication such as digoxin is given to patients with heart failure, to improve myocardial contraction and reduce the heart rate. Salbutamol, used to control the symptoms of asthma, can cause tachycardia.
Assessing the pulse
The radial pulse can be found at the inner aspect of the wrist below the base of the thumb and medial to the radius, or wrist bone. It is palpated by placing two fingers, usually the index and third, and applying gentle pressure on the radial artery (see Fig. 14.9 ). Measuring the pulse is described in Box 14.16 . The regularity and strength are also assessed (see below). Radial, popliteal and pedal pulses may be difficult to locate in adults who are cold or when the environment is cold and those with:
• Peripheral vascular disease, which impairs peripheral circulation
• Low blood pressure (hypotension, see Ch. 17 )
• Cardiac arrhythmias (see Ch. 17 )
• Peripheral oedema (see Chs 17 , 19 ).
When counting the pulse rate, the regularity is also noted, as this reflects the cardiac rhythm. Normally the rhythm is regular as the heart contracts regularly. However, young people may have a rhythm disturbance, known as sinus arrhythmia, which alters with inspiration and expiration. People who have heart disease may have an irregular rhythm due to disordered electrical conduction within the heart, e.g. atrial fibrillation (see Ch. 17 ). Heart irregularities can be investigated through an electrocardiogram (ECG) (see Ch. 17 ) and an irregular rhythm should always be reported immediately.
The force of the pulse is also assessed. The terms used to describe force or volume are:
• Normal – the pulse is easy to feel
• Bounding – pulse feels ‘springy’ due to an increase in force of cardiac contraction or circulating blood volume; usually found in the presence of infection
• Thready – pulse feels weak, difficult to palpate and difficult to count, which may be due to dehydration or haemorrhage
• Absent – indicates a blockage of the palpated artery or, together with other observations such as skin colour, cardiac arrest.
Factors that influence the force of the pulse include the circulating blood volume and the action of hormones on blood vessel walls causing vasoconstriction or vasodilatation.
The pulse reading is recorded on the clinical observation chart and contributes to the Early Warning Score (see Fig. 14.14 , p. 333 ).
Features of the pulse in newborns, infants and children
Pulse rates in children vary with age; normal ranges are shown in Table 14.4 . The pulse can be palpated over the radial, brachial or femoral artery. The pulse rate should be assessed while a baby or child is asleep or at rest as crying, eating or sucking increase heart rate.
Apical pulse
The apical pulse is a central measurement, which is the most common method of recording heart rate in infants and young children and also in adults who may have heart disease with rhythm disturbances. The apical (apex) beat is located at the apex of the heart. Measurement of the apex/radial pulse in adults is explained in Chapter 17 .
The apical pulse is detected using a stethoscope and listening to heart sounds at the apex of the heart (the pointed end of the ventricle). In children, placement of the stethoscope is dependent on age. The stethoscope is placed:
• At the 4th intercostal space inside the nipple in children under 5 years of age
• At the 5th intercostal space at or inside the nipple for children over 5 years old ( Trigg & Mohammed 2010 ).
Blood pressure
This section outlines what blood pressure (BP) is and the factors that affect it in health; for more detail you should consult your physiology textbook. The equipment needed and how to measure BP are explained. It is important to be familiar with the early material in this section before attempting to practise BP measurement.
BP corresponds to the pressure exerted on arterial walls as blood moves through them. BP measurements provide information about cardiovascular status, which can assist in the diagnosis of disease or evaluation of treatment. Two measurements are made and usually recorded in millimetres of mercury (mmHg):
• Systolic pressure, which represents the greatest pressure in the main arteries following contraction of the left ventricle
• Diastolic pressure, which is the lowest pressure in the main arteries and occurs at the end of ventricular relaxation while the heart is at rest, before the next cardiac contraction.
The convention for writing blood pressure is to put the systolic pressure first and then the diastolic, e.g. 120/70 mmHg.
Factors that determine blood pressure
BP is determined by several factors including the cardiac output, venous return, blood volume, peripheral vascular resistance (the resistance within arteries and arterioles) and elasticity of large arteries. BP is dynamic, and so varies over the course of the day depending on body demands. For more detail about factors that determine BP and its control, you should consult your physiology textbook.
Blood pressure values
Adult BP is normally in the range of 100–130 mmHg systolic and 60–90 mmHg diastolic. The National Clinical Guideline Centre (NCGC) recommends that optimal BP should be <120/<80 ( NCGC 2011 ). Table 14.5 shows normal BP values for children.
Normal BP values for children
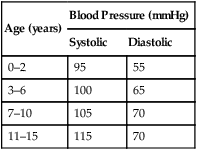
(Reproduced with permission from Hull, D., Johnston, D.I., 1999. Essential paediatrics, fourth ed. Churchill Livingstone, Edinburgh.)
Hypertension (high blood pressure) is defined as systolic blood pressure >140 mmHg or diastolic blood pressure >90 mmHg. The NCGC (2011) recommends that hypertension should be confirmed using 24-hour ambulatory blood pressure monitoring (ABPM) rather than being solely based on measurements taken in the clinic; the use of ABPM is predicted to be more cost-effective for the NHS. Guidance is also provided for home blood pressure monitoring (HBPM) which empowers people to become more involved in the monitoring and management of their hypertension ( NCGC 2011 ).
Hypotension describes BP lower than the normal range of 100 mmHg systolic and/or 60 mmHg diastolic. Hypertension and hypotension are explored further in Chapter 17 .
Equipment used for BP measurement
BP is usually measured by non-invasive means, using either the auscultatory or electronic method. The equipment required includes a sphygmomanometer, which may be aneroid or electronic, and an appropriately sized cuff ( Table 14.6 ). BP is sometimes continuously monitored through the invasive method using a catheter inserted into an artery, a technique beyond the scope of this book that is confined to the care of critically ill people.
Estimated BP cuff sizes
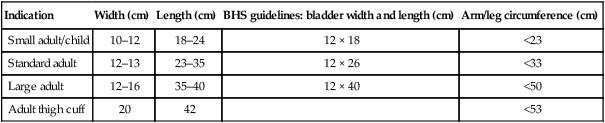
(Reproduced with permission from British Hypertension Society, 2011 . How to measure blood pressure. Online. Available: www.bhsoc.org September 2011.)
Sphygmomanometers
Mercury sphygmomanometers were used for many years; however, health and safety concerns regarding the use and disposal of mercury in the workplace have emerged and therefore these may no longer be in use in practice. Increasingly common methods of BP measurement are the use of aneroid or electronic sphygmomanometers ( Fig. 14.10 ).
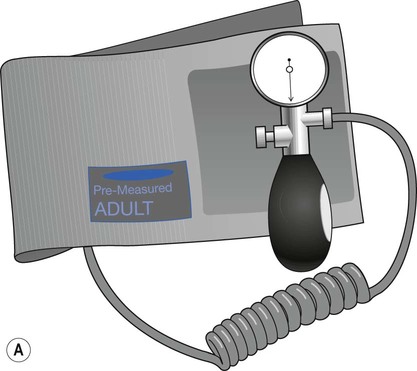
Aneroid sphygmomanometers are less bulky and more portable than other types. They do not use mercury and are a safe alternative that has quickly gained acceptance. However, they have been found to be less reliable as they often underestimate BP. These are not recommended for use in hospitals because they rapidly deteriorate due to high usage and also need frequent calibration to ensure their accuracy ( NCGC 2011 ).
Electronic sphygmomanometers include a pressure sensor within the cuff that registers the systolic and diastolic pressures, which are then displayed digitally. The advantages of these machines are that they require little instruction, eliminate observer bias, and can also display heart rate, mean BP, and the time and date, simultaneously. However, they are often very sensitive to movement and can still be inaccurate in patients with irregular heart rhythms such as atrial fibrillation. No stethoscope is needed and therefore this is not an auscultatory method of BP measurement.
BP measurements may be influenced by a range of factors and all forms of non-invasive BP monitoring have limitations ( Box 14.17 ).
How reliable is non-invasive BP measurement?
BP is often recorded on a single occasion and one-off readings do not necessarily reveal trends of a person's BP.
• Variability over the day: BP varies over the course of a day in order to meet different requirements such as exercise and other activities, e.g. eating, sleeping, smoking.
• White coat syndrome: This is an increase in BP ascribed to anxiety or anticipation of BP measurement by healthcare professionals.
• Postural hypotension: This is a drop in BP that occurs when standing up from a lying position. It is fairly common in older adults and people receiving antihypertensive medication. In this situation, BP should be measured in both lying and standing positions.
• Arrhythmias: Irregular heart rhythms may result in variations in the sounds heard from beat to beat as well as differences in the time between each beat. As a consequence, recordings made using the auscultatory method can be inaccurate.
• Pregnancy: BP is monitored closely during pregnancy as hypertension can have serious consequences. In addition, BP can fall when lying supine if the fetus obstructs the inferior vena cava, reducing venous return.
• Observer error: The wrong technique or faulty equipment can lead to inaccurate readings.
1. Access the National Clinical Guideline Centre and read Clinical Guideline 127 and identify some of the factors that contribute towards a loss of accuracy when measuring BP.
2. BP equipment is frequently used in placements and needs regular checks to ensure that measurements will be accurate. In your placement:
• Identify the type(s) of sphygmomanometer used.
• Find out how often they are calibrated and how this is carried out.
• Identify the different sizes of BP cuffs available and whether they are suitable for use with all the patients/clients there (see Table 14.6 ).
• Find out when and how they are cleaned.
• Examine the cuffs for signs of wear and tear. If they are in need of repair, discuss the further actions required with your mentor.
National Clinical Guideline Centre. Hypertension: Clinical management of primary hypertension in adults. Online. Available www.nice.org.uk/nicemedia/live/13561/56007/56007.pdf , 2011. [September 2012].
Some BP cuffs are supplied in two separate parts: the cover (or sheath) and an inner inflatable bladder. Both components should be inspected before use. The cuff should be clean and intact. The tubing attached to both the sphygmomanometer and the inflation bulb should also be intact with no leaks or signs of perishing.
It is important to use the correct size of BP cuff, irrespective of the type of sphygmomanometer used (see Table 14.6 ). The bladder within the cuff should encircle at least 75–80%, but not more than 100%, of the upper arm. The width of the cuff should be more than 50% of the length of the upper arm. An underestimation of BP will be recorded if the cuff is too large; overestimation of BP will occur if the cuff is too small ( NCGC 2011 ).
Measuring BP
The important points are explained here and BP measurement is outlined in Box 14.18 . BP readings are entered on the clinical observation chart and contribute to the calculation of the Early Warning Score (see Fig. 14.14 , p. 333 ).
Measurement of BP
• A sphygmomanometer (see p. 328 )
• An appropriately sized cuff (see Table 14.6 )
• A stethoscope for auscultatory methods
• An observation chart ( Fig. 14.14 , p. 333 ) or medical/nursing notes.
• Wash hands as per local policy
• BP measurement should be explained, including the feeling of ‘tightness’ in the arm, and verbal consent obtained; maintain respect and dignity at all times
• The person should be seated, lying supine for at least 5 minutes, or standing for 1 minute before the procedure begins. They should be relaxed and not moving or speaking
• The arm is supported at the level of the heart (mid sternum) and held straight but relaxed, ensuring that no tight clothing constricts the arm
• The cuff (see below) is applied:
• with the centre of the bladder marked on the cuff over the brachial artery (see Fig. 14.11 )
• with the lower edge of cuff 2–3 cm above pulsation of the brachial artery
• in aneroid sphygmomanometers so that the tubing emerges ‘up the arm’ as movement of the tubing across the antecubital fossa can create artefactual sounds.
Measurement using an aneroid sphygmomanometer
• Estimate the systolic pressure beforehand by:
• palpating the brachial artery
• inflating the cuff using the bulb until pulsation disappears
• deflating cuff until pulsation is felt; the point at which pulsation appears is an estimate of the systolic pressure
• Then inflate the cuff to 30 mmHg above the systolic level, estimated earlier; at this point the brachial pulse will no longer be felt
• Place the diaphragm of the stethoscope over the brachial artery and slowly deflate the cuff at a rate of 2–3 mm/s until you hear regular tapping sounds – this is phase 1, the systolic pressure (see Fig. 14.12 )
• Systolic pressure and diastolic pressure are recorded to the nearest 2 mmHg
• Measure diastolic pressure – phase 4 (see Fig. 14.12 ): abrupt muffling sounds become soft and blowing in quality just before the sounds disappear (phase 5) – this point is recorded as the diastolic pressure
• Completely deflate and remove the cuff to prevent any further compression of the limb
• It may be necessary to repeat the procedure for both lying and standing positions
• Clean the diaphragm of the stethoscope according to local policy
• Record the pressures heard as soon as possible after assessment, noting the position of the patient/client (lying, standing or sitting down) and the arm used. This may be on an observation chart (see Fig. 14.14 , p. 333 ) or in the notes
Notes: NCGC (2011) recommends that pressures in both arms should be recorded on the first visit and that the arm with the highest BP should be used in subsequent measurements.
British Hypertension Society. How to measure blood pressure. Online. Available www.bhsoc.org/resources/how-to-measure-blood-pressure/ , 2011. [September 2012].
National Clinical Guideline Centre. Hypertension. Clinical management of primary hypertension in adults. Clinical Guideline. Online. Available www.nice.org.uk/nicemedia/live/13561/56007/56007.pdf , 2011. [September 2012].
Measuring BP in newborns, infants and children
Although BP may be measured less frequently in children than in adults, consideration must be given to the following:
• It is hard to auscultate the antecubital fossa pulse, so an electronic blood pressure machine should be used in babies and young children
• The lower edge of cuff should be close to the antecubital fossa
• BP should be recorded when a baby is asleep or resting. Crying, sucking and eating increase BP
• Allay any anxiety before measurement. Young children may feel more secure if BP is taken while sitting in a parent's lap.
Further information can be found in Trigg and Mohammed (2010) .
Inflating the cuff
Inflation of the cuff compresses the brachial artery (see Fig. 14.11 ) and the cuff is inflated automatically when using an electronic sphygmomanometer. When an aneroid sphygmomanometer is used, the bladder inside the BP cuff is attached to an inflation bulb with a release valve, which allows the cuff to be inflated manually.
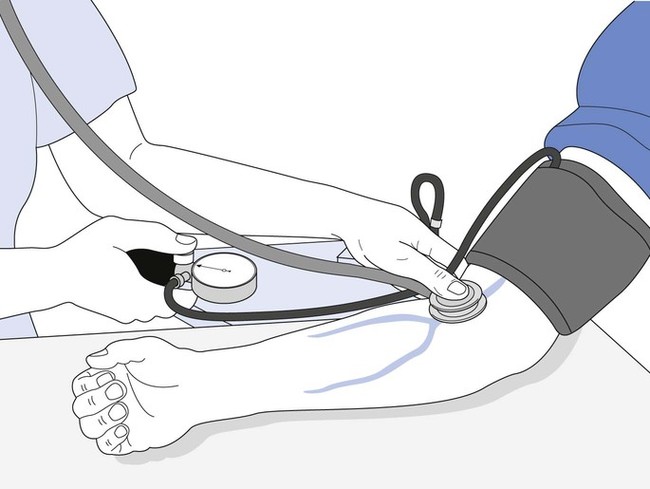
Korotkoff sounds
The auscultatory method relies on the detection of a series of sounds. When using an aneroid sphygmomanometer, a stethoscope with clean, well-fitting earpieces is required. Earpieces are placed in the ears pointing towards the nose. The diaphragm is placed on the brachial artery in the antecubital fossa ( Fig. 14.11 ) to listen to sounds in the brachial artery. These are known as Korotkoff sounds, which are divided into five phases ( Fig. 14.12 ). The first phase can be heard as a clear tapping noise via the stethoscope as the cuff is deflated. This is the systolic blood pressure and represents phase 1. Muffled whooshing noises are usually heard during phases 2 and 3. The sound becomes much more muffled and softer during phase 4 before it disappears at phase 5. The diastolic pressure is normally recorded at the end of phase 4. However, if the sounds continue until 0 mmHg, then the point at which the sounds change at phase 4 is recorded.
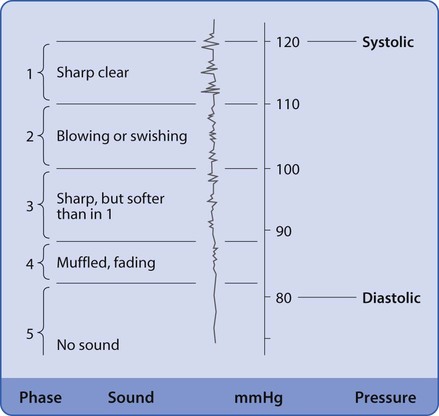
Assessing respirations
The accuracy and frequency of recording of respirations is very important. Respiratory rate recording has been shown to be a crucial indicator of serious deteriorations in health status. Decreases in the respiratory rate (<8 breaths/min) and depth have been noted in the hours preceding cardiopulmonary arrest. It has also been suggested that assessment of respiratory rate is not performed as accurately or as frequently as it should be. Additionally, there appears to be an over-reliance on the use of peripheral oxygen saturation monitors to determine respiratory function ( Hogan 2006 ; NICE 2007 ). However, both respiratory rate and peripheral oxygen saturation are required to calculate the EWS. Analysing and assessing respiratory status requires the observation of several factors, which are outlined below.
At rest, breathing should be regular, effortless and quiet. However, exercise or breathing difficulties may alter the rate, depth, rhythm and/or sound of breathing. Rate and depth of respirations may also change as a result of pain, pyrexia, emotional states and body position, as well as breathing difficulties such as ‘shortness of breath’ (dyspnoea). They are also influenced by the use of drugs such as nicotine in cigarettes, and opioids, e.g. morphine (see Ch. 23 ), as well as cocaine and amphetamines. Assessment of respirations is described in Box 14.19 .
• The patient should be comfortable and relaxed
• Unusually, the patient is not informed that their respirations are going to be counted
• Accuracy and reliability of measurements are increased by counting for a full minute
• Respiratory rate is recorded over 1 minute by observing the rise and fall of the chest wall. If breathing is shallow, it may be easier to count movements using a hand placed lightly on the chest or abdominal wall although the patient may be aware of this
• Each cycle is counted discreetly ( Fig. 14.13 ), usually after taking the pulse

• Other factors also assessed at this time include:
• Respiratory rhythm (see p. 332 )
• Depth of breathing (see p. 332 )
• Effort of breathing, e.g. use of accessory muscles (see p. 332 )
• Noises associated with breathing (see p. 332 )
• Patient's colour, e.g. presence of cyanosis (see Ch. 17 )
• Presence of cough or production of sputum (see Ch. 17 )
• The respiratory rate is recorded on the observation chart (see Fig. 14.14 ) or patient/client notes
• Any abnormal findings are reported and recorded in the notes.
Respiratory rate
Breathing occurs in cycles. The first phase is inspiration, which is followed by a short pause before expiration (see Ch. 17 ). The rate and depth of breathing are controlled by the respiratory centre located in the medulla oblongata. Blood levels of carbon dioxide (CO 2 ) and oxygen (O 2 ), as well as pH (acidity), are the main influences on respiratory rate. Chemoreceptors located in the brain stem, carotid arteries and the aortic arch monitor and respond to changes in the blood levels of CO 2 , O 2 and pH. An increase in blood carbon dioxide levels (PaCO 2 ) and a fall in blood pH (increased acidity) activate the chemoreceptors that respond by increasing the respiratory rate, which increases the elimination of CO 2 and raises blood pH. Breathing can also be influenced by external factors such as pain, emotion or voluntary control. For more information about breathing and its control, you should consult your physiology textbook.
Counting respiratory rate in adults
Respiratory rate is the number of respirations per minute and is recorded as RR. In adults, the normal rate is 12–18 respirations/min. Tachypnoea describes a respiratory rate that exceeds 20/min; absence of breathing is known as apnoea. The respiratory rate is entered on the observation chart (see Fig. 14.14 , p. 333 ) and its calculation into the Early Warning Score (EWS).
Counting respiratory rate in infants and small children
In babies under 12 months old, it is recommended that a stethoscope is used to listen to air movement in the lungs to count the breaths per minute. Average respiratory rates for children are shown in Table 14.7 . The child should be relaxed and quiet before measurement is made by lightly placing a hand on their abdomen to count the breaths. If this is not possible, it may be necessary to observe breathing while the child is quietly interacting with a parent or playing.
Children's average respiratory rates
Respiratory rhythm
Breathing is usually regular in healthy adults. It may be described as regular or irregular and can be influenced, e.g. by emotions such as fear or crying and during breath-holding or panic attacks. Babies often have a less regular rhythm, possibly due to incomplete development of the normal respiratory control systems (see Ch. 17 ).
Abnormal respiratory rhythms
Alterations in rhythm can also be observed in patients with neurological dysfunction that has impaired the respiratory centre within the brain stem.
Damage or poor blood supply to the brain stem can result in an irregular rhythm and rate called Cheyne–Stokes breathing. In this condition, breathing patterns change between shallow and slow and deep and rapid, with varying periods of apnoea in between. This type of breathing is often present at the end-of-life.
Depth of breathing
The depth of a breath is determined by the volume of air inhaled. In healthy adults, during relaxed breathing, this is about 500 mL and is called the tidal volume. This and other indicators of respiratory status may also be measured by nurses, especially in people with chronic respiratory conditions such as chronic bronchitis and asthma (see Ch. 17 ).
The depth of breathing is described as normal, shallow or deep and is observed by watching the rise and fall of the chest wall. These are, however, subjective observations and so open to interpretation. Expansion of both sides of the chest should be the same, i.e. ‘equal’.
The term hypoventilation is used to describe shallow slow breathing, which implies limited chest movement. Hyperventilation is used to describe fast and deep breathing, and considerable movement of chest wall may be observed.
Deep, regular breaths may be ‘Kussmaul’ respirations, caused by an increase in blood acidity (low blood pH). This can arise as a result of uncontrolled diabetes.
Effort of breathing
Normally, at rest, breathing is regular, effortless and quiet. During exercise, the breathing pattern becomes more active as body oxygen demand rises and blood carbon dioxide levels increase (hypercapnia). Exercise requires the movement of more air into and out of the lungs, more quickly and forcibly, and also employs the accessory muscles of respiration, i.e. the internal intercostal muscles and the muscles in the neck and shoulders. Forced expiration is facilitated by the abdominal muscles contracting and pushing the diaphragm upwards. Expiration is no longer passive, but becomes forced.
Noises associated with breathing
Although breathing is normally quiet, alterations to breathing patterns can also include changes to the sound of breathing. Whistling noises called wheezing due to constriction of the airways can be heard on expiration in people with chronic lung disease such as bronchitis or asthma. Obstruction of the larynx results in high-pitched noises during inspiration, which are termed stridor.
Children experiencing breathing difficulties can also develop associated vocal noises such as grunting, wheezing and stridor. In addition, they may hold themselves rigidly, have a retracted neck and nasal flaring ( Trigg & Mohammed 2010 ).
Early Warning Score (EWS)
For patients who are acutely ill and at risk of developing a critical illness, vital sign recordings should be entered onto an EWS, Modified Early Warning Score (MEWS) or Track and Trigger chart. Those who are at high risk of deterioration include all patients admitted as an emergency, have a chronic health problem, have had surgery and those whose condition may be causing concern or is unstable. However, NICE (2007) recommends that all acute hospital in-patients should have their vital signs recorded and monitored via a track and trigger system. The Royal College of Physicians (2012) has advocated using a standardized NHS National Early Warning Score (NEWS) chart within a year.
The respiratory rate, pulse, systolic blood pressure and body temperature are entered on the EWS chart and awarded a score. Additional information that is scored and required for an EWS includes the patient's hourly urine volumes (see Ch. 20 ), the Glasgow Coma Score (GCS) or Level of response (AVPU) (see Ch. 16 ) and the oxygen saturation percentage (SpO 2 ) (see Ch. 17 ). The score is calculated by rating each parameter and recording it on the EWS chart ( Fig 14.14 ).
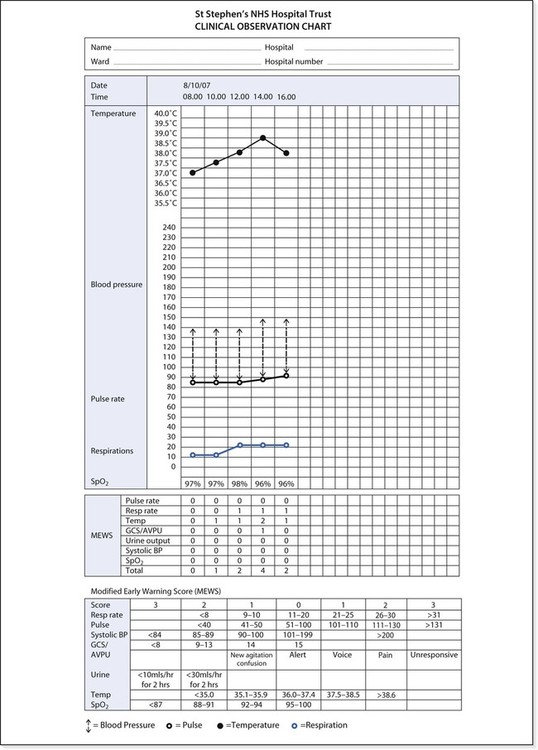
Calling criteria
Once the EWS score is calculated, the assessor is directed towards making a decision about what to do next. This might be to:
• Increase the frequency of patient observations, monitor trends and inform the nurse in charge
• Communicate the results to a senior nurse if the score is 3 in any one category
• Contact the critical care outreach team and the senior nurse to assist in managing the patient's condition if the score is 4 or above or increasing by 2 or more or the GCS falls by 2 or more or if the patient's condition is a cause for concern ( NICE 2007 ).
Height and weight
Measurement of height and weight should be made on admission to hospital or as part of a community assessment. Extremes of weight are associated with health risks. Body mass index (BMI, see Ch. 19 ) is a useful guide to whether an adult's body weight is appropriate for their height. Knowledge of people's height and weight is needed to calculate drug doses, including anaesthetics, and fluid and nutritional requirements, especially in children.
Children may also be regularly weighed and measured to monitor growth rates and weight gain, which are important in monitoring their health and development. In the UK, children's weight and height should be recorded on the appropriate centile chart produced by the Royal College of Paediatrics and Child Health (2009) .
Measuring body weight requires the use of electronic calibrated scales and is recorded in kilograms (kg). A child under the age of 2 should have all clothing removed and placed on scales. Children over 2 years old should have underwear on and asked to sit or lie or stand on the scales.
If serial measurements are made, this should be at the same time each day or week and in similar clothing. Daily weight may be recorded to assess, e.g. fluid loss in response to diuretic drugs. When weight loss is a goal, e.g. in obesity, weight may be monitored weekly.
Children are measured to the nearest centimetre and metres are used for adults; e.g. 65 cm for a child and 1.65 m (165 cm) for an adult.
A fixed measure is used for adults and children over the age of 2 years, standing with the back against a wall or scale. The head should be in the midline and the heels, buttocks and backs of shoulders should touch the wall. A moveable rod is placed on the top of the head, to assist in reading the measurement. For children under 24 months, length is measured instead of height. The child is placed on their back and their head is gently held in the midline. The knees should be held and pushed down until the legs are flat on the table and the child's body is extended ( Fig. 14.15 ). Length, in centimetres (cm), is measured using a measuring tape. In children, the circumference of the head, chest and abdomen may also be measured.
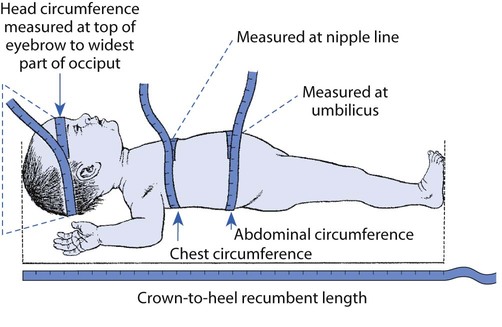
Key words and phrases for literature searching
Assessment tool
Early Warning Score
Body core temperature
Hypothermia
Nursing history
Nursing model
Nursing process
Person-centred care
Sphygmomanometer
Tachycardia
Thermometry
Useful websites
British Hypertension Society www.bhsoc.org
Tidal model www.tidal-model.com
Waterlow scale www.judy-waterlow.co.uk
National Clinical Guideline Centre www.ncgc.ac.uk
All websites accessed September 2012.
- Undergraduate
- Bachelor of Science in Nursing
- Professional Nursing Pathways Program
- Registered Nurse to Bachelor of Science in Nursing
- Registered Nurse to Master of Science in Nursing
- Registered Nurse to Master of Science in Nursing – Family Nurse Practitioner
- MSN in Nursing Administration
- MSN in Nursing in Education
- MSN in Adult Gerontology Acute Care Nurse Practitioner
- MSN in Adult Gerontology Primary Care Nurse Practitioner
- MSN - Family Nurse Practitioner
- MSN in Pediatric Acute Care Nurse Practitioner
- MSN in Pediatric Primary Care Nurse Practitioner
- Doctor of Nursing Practice
- Post-Baccalaureate
- Post-Baccalaureate Certificate in Nursing Administration
- Certificate in Nursing Education
- Post-Master's
- Adult Gerontology Acute Care Nurse Practitioner Certificate (Post Master’s)
- Adult Gerontology Primary Care Nurse Practitioner Certificate (Post Master’s)
- Family Nurse Practitioner Certificate (Post Master’s)
- Pediatric Acute Care Nurse Practitioner Certificate (Post Master’s)
- Pediatric Primary Care Nurse Practitioner Certificate (Post Master’s)
- Post-Master’s Certificate in Nursing Administration
- Bachelor of Science in Public Health
- View All Programs
- Online Experience
- Academic Calendar
- About CONHI
- Student Services
- Student Testimonials
- Faculty Profiles
Related Articles
Welcome to our website! How did you hear about us? Take Survey »
Home > Online Programs > RN to BSN > What Is a Holistic Health Assessment?
What Is a Holistic Health Assessment?
- Published On: September 30, 2024
The health assessment is a key nursing duty that impacts a patient’s overall care and health outcomes. Although nurses routinely perform traditional assessments, they often have minimal experience with holistic health assessments.
However, holistic health assessments play an essential role in determining an effective treatment plan, as evidenced by coursework in the CCNE-accredited online Registered Nurse (RN) to Bachelor of Science in Nursing (BSN) program from The University of Texas at Arlington (UTA). The following is a look at holistic assessments, their benefits and pathways to learning more about their successful application.
How Are Holistic Health Assessments Different?
Most nurses have significant experience performing standard health assessments that are both comprehensive and problem-focused. Through patient interviews and physical exams, both standard and holistic assessments include a review of:
- Past personal medical history, including prior hospitalizations, illnesses and surgeries
- Family history, such as general health, history of illness and cause of death
- Food, environmental and medication allergies, plus type and extent of reaction(s)
- Prescription and over-the-counter medication history, including dosages and routes of administration
- Location and severity of pain
- Evaluation of fall risks
- Mental health, including signs of confusion, depression, substance abuse and suicidal ideations
- Vital signs such as heart rate, blood pressure, temperature and oxygen saturation
However, in a holistic health assessment — a central component of holistic nursing — a nurse typically dives deeper into a patient’s health history, spending more time and energy gathering information and identifying patterns or root causes. Additionally, holistic assessments emphasize the following:
- Person-centered care. Traditional assessments tend to be problem-focused, largely using the information-gathering session to discuss the most acute medical issue, or “chief complaint.” Holistic assessments use a person-centered approach and include an extensive evaluation of the patient’s physiological, psychological, sociological, developmental, spiritual and cultural status. The conversation covers these topics as well as lifestyle choices and habits such as exercise, nutrition and sleep.
- Mutual goal setting. As part of a holistic health assessment, the nurse and patient work together to establish wellness goals. Instead of prescribing a medication or treatment plan, the nurse suggests tools and methods that may help achieve those goals, and the patient determines the best strategies to adopt. Patient engagement and involvement in the decision-making process are critical to this empowering component of the holistic health assessment.
Importantly, holistic assessment is no longer a fringe or alternative concept. Large nursing organizations now incorporate components of holistic assessment practices — and holistic nursing practices in general — into overarching nursing process descriptions and guidelines.
For instance, person-centered care is the second domain (out of 10) of the Essentials from the American Association of Colleges of Nursing (AACN) — the organization’s outline of curriculum content and expected competencies for nursing program graduates. In addition, the American Nurses Association (ANA) states, “Assessment includes not only physiological data, but also psychological, sociocultural, spiritual, economic, and life-style factors as well.”
What Are the Benefits of Holistic Health Assessments?
Holistic nursing assessments seek to understand the unique challenges, strengths and goals of each patient. Some of the many benefits of this approach include:
- Increased communication. By working together to establish goals and discussing options for the best course forward, nurses and patients increase their communication and create more balanced, collaborative interactions.
- Patients feel valued. Many patients struggle with making long-term, healthful changes, especially if they feel unheard or treated as just a number. Holistic assessments recognize all patients as individuals by respecting their beliefs and values and encouraging them to actively craft goals and care plans.
- Improved outcomes. Helping patients gain more control over their healthcare decisions can expedite their adoption of positive lifestyle changes and strengthen treatment plan adherence — all of which may lead to improved outcomes.
Where Can Nurses Learn More About Holistic Methods?
The U.S. Bureau of Labor Statistics (BLS) projects employment of registered nurses will increase by 6% between 2023 and 2033, faster than the average growth for all occupations. Further, the use of complementary and alternative medicine is growing rapidly. Research shows that evidence-based complementary and alternative medicine therapies can be very impactful in treating diseases.
Holistic methods exist at this intersection of evidence-based practice and complementary and alternative medicine. As such, holistic health practices are becoming a foundational component of nursing education. To meet the demand, nurses interested in pursuing holistic care may benefit from more detailed instruction. UTA’s online RN to BSN program includes a course dedicated to the application of holistic health assessments across the patient lifespan.
While nurses still use traditional health assessments, there is a rapidly growing interest in holistic care. Nurses skilled in holistic health assessments can work closely with their patients to identify goals and create sustainable care plans that move them toward more robust wellness.
Learn more about UTA’s online RN to BSN program .
Request More Information
Submit this form, and an Enrollment Specialist will contact you to answer your questions.
*All fields required.
- Program of Interest * Program of Interest* BS in Public Health Adult Gerontology Acute Care Nurse Practitioner Certificate Adult Gerontology Primary Care Nurse Practitioner Certificate BSN Certificate in Nursing Education DNP FNP Certificate MSN in Adult Gerontology Acute Care Nurse Practitioner MSN in Adult Gerontology Primary Care Nurse Practitioner MSN in Nursing Administration MSN in Nursing Education MSN in Pediatric Acute Care Nurse Practitioner MSN in Pediatric Primary Care Nurse Practitioner MSN – Family Nurse Practitioner Pediatric Acute Care Nurse Practitioner Certificate Pediatric Primary Care Nurse Practitioner Certificate Post-Baccalaureate Certificate in Nursing Administration Post-Master’s Certificate in Nursing Administration Professional Nursing Pathways Program RN to BSN RN to MSN RN to MSN – Family Nurse Practitioner
- First Name *
- Last Name *
- How did you hear about us? * How did you hear about us?* Coworker Email Employer Family/Friend Information Session Magazine/Newspaper Online Professional Organization Radio/TV
- Email This field is for validation purposes and should be left unchanged.
Or call 866-489-2810
By submitting this form, I am providing my digital signature agreeing that The University of Texas at Arlington (UTA) and its agent, Risepoint, may email me or contact me regarding educational services by telephone and/or text message utilizing automated technology or a pre-recorded message at the telephone number(s) provided above. I understand this consent is not a condition to attend UTA or to purchase any other goods or services. Privacy Policy . SMS Terms .
Ready to Begin?
Start your application today!
The University of Texas at Arlington | 701 S. Nedderman Drive, Arlington, TX 76019 | 817-533-3118 or 866-489-2810 817-533-3118 or 866-489-2810
Privacy Policy
Terms & Conditions
Course Login
© 2024 The University of Texas at Arlington
Risepoint maintains this website on behalf of The University of Texas at Arlington. UTA maintains responsibility for curriculum, teaching, admissions, tuition, financial aid, accreditation, and all other academic and instruction-related functions and decisions. Learn more about Risepoint .
Call 866-489-2810
- Social Media
- Direct mail
- Search Engine
- Event/Conference
- This is my first time
- Within the last 30 days
- 1-2 months ago
- 3+ months ago
Request Information
- Phone This field is for validation purposes and should be left unchanged.

IMAGES
COMMENTS
Jan 31, 2023 · That is the vision of a holistic needs assessment, a powerful tool that goes beyond surface-level evaluations to truly understand and address the complexities of an individual’s life. Holistic assessment in nursing is a comprehensive and holistic approach to evaluating a patient’s overall health and well-being.
5 days ago · Pursuing a degree with coursework in holistic nursing can also help you learn to incorporate holistic nursing practices in your career. 6. Steps to conducting a holistic assessment in nursing. A holistic assessment is a patient-centered tool for developing a treatment plan based on evidence-based practices, patient values, and nursing intuition.
Something I love about holistic nursing is that it is an approach to care that is focused on preventing illnesses and diseases as much as it is about finding cures for them. When we implement holistic nursing measures, we teach our patients ways of living healthy which can prevent some illnesses and diseases and promote better health and outcomes.
Sep 5, 2024 · Holistic assessment in nursing is a comprehensive approach to evaluating a patient’s overall health and well-being. It goes beyond traditional methods by considering various aspects that may impact a person’s health , including physical, mental, social, financial, and environmental factors .
Feb 22, 2024 · At its core, holistic health is a comprehensive approach to nursing care that assesses the patient as a whole rather than focusing only on specific symptoms or medical diagnoses. Holistic health assessments allow nurses to understand a patient’s overall well-being by considering the many factors influencing their health.
In summary, the combination of the NP (Melin-Johansson et al, 2017), MoN (Roper et al, 2008) alongside assessment tools and nursing skills are fundamental key aspects to a successful holistic care plan. This combination ensures a full assessment of a patient’s holistic care needs and indicates appropriate multidisciplinary interventions.
As assessment is the cornerstone of establishing what a person's needs are, so the quality of assessment is pivotal to the success of the nursing process. Successful nursing intervention hinges on a complete and thorough assessment being undertaken.
Apr 18, 2018 · A holistic health assessment allows the nurse to gain information essential for diagnosis, planning and implementation. It shows respect for the patient’s preferences and preserves the patient’s dignity. The six aspects of a holistic assessment include: Physiological: Complete a physical assessment.
Sep 30, 2024 · However, in a holistic health assessment — a central component of holistic nursing — a nurse typically dives deeper into a patient’s health history, spending more time and energy gathering information and identifying patterns or root causes. Additionally, holistic assessments emphasize the following: Person-centered care.
Dec 13, 2023 · Holistic nursing is a nursing specialty based on holistic healthcare principles. The patient-centered approach is grounded in empathy, compassion and respect and considers each patient’s unique values, beliefs and cultural background. Nurses gather this information by performing a holistic health assessment that helps inform diagnosis ...