Evidence Based Nursing Practice
- Articles & Journals
- Searching the Literature

Contact the Library
All Mayo staff with LAN IDs and passwords can use Document Delivery to receive copies of journal articles and book chapters.
If you require additional assistance, please contact the Library .
Evidence Based Practice Resources
- Mayo Clinic Evidence Based Practice

Systems - integration of evidence with patient records Summaries - practice guidelines found via Clinical Key & UpToDate Synopses of Syntheses - focused journals: Evidence-Based Nursing , Evidence-Based Medicine , ACP Journal Club Syntheses - m eta-analyses, systematic reviews and other evidence syntheses found through Cochrane , CINAHL , PubMed Synopses of Single Studies - focused journals: Evidence-Based Nursing , Evidence-Based Medicine , ACP Journal Club Single Studies - CINAHL , PubMed
- See McMaster University Nursing 6S Pyramid for additional details
Nursing Research Journals
Log-in to Current Awareness to get contents pages delivered to your e-mail!
- Current Awareness - Nursing Research Journals
Recent Articles from the CINAHL Database
- Next: Books >>
- Last Updated: Nov 20, 2023 3:07 PM
- URL: https://libraryguides.mayo.edu/evidencebasednursing
Evidence-based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review
Affiliations.
- 1 Helene Fuld Health Trust National Institute for Evidence-Based Practice in Nursing & Healthcare, College of Nursing, The Ohio State University, Columbus, Ohio, USA.
- 2 St. John Fisher University, Wegmans School of Nursing, Rochester, New York, USA.
- 3 Sinai Hospital, Baltimore, Maryland, USA.
- 4 Summa Health System, Akron, Ohio, USA.
- 5 The Ohio State University, College of Nursing, Columbus, Ohio, USA.
- 6 Memorial Sloan-Kettering Cancer Center, New York, New York, USA.
- 7 Family CareX, Denver, Colorado, USA.
- 8 Affiliate Faculty, VCU Libraries, Health Sciences Library, Virginia Commonwealth University School of Nursing, Richmond, Virginia, USA.
- PMID: 36751881
- DOI: 10.1111/wvn.12621
Background: Evidence-based practice and decision-making have been consistently linked to improved quality of care, patient safety, and many positive clinical outcomes in isolated reports throughout the literature. However, a comprehensive summary and review of the extent and type of evidence-based practices (EBPs) and their associated outcomes across clinical settings are lacking.
Aims: The purpose of this scoping review was to provide a thorough summary of published literature on the implementation of EBPs on patient outcomes in healthcare settings.
Methods: A comprehensive librarian-assisted search was done with three databases, and two reviewers independently performed title/abstract and full-text reviews within a systematic review software system. Extraction was performed by the eight review team members.
Results: Of 8537 articles included in the review, 636 (7.5%) met the inclusion criteria. Most articles (63.3%) were published in the United States, and 90% took place in the acute care setting. There was substantial heterogeneity in project definitions, designs, and outcomes. Various EBPs were implemented, with just over a third including some aspect of infection prevention, and most (91.2%) linked to reimbursement. Only 19% measured return on investment (ROI); 94% showed a positive ROI, and none showed a negative ROI. The two most reported outcomes were length of stay (15%), followed by mortality (12%).
Linking evidence to action: Findings indicate that EBPs improve patient outcomes and ROI for healthcare systems. Coordinated and consistent use of established nomenclature and methods to evaluate EBP and patient outcomes are needed to effectively increase the growth and impact of EBP across care settings. Leaders, clinicians, publishers, and educators all have a professional responsibility related to improving the current state of EBP. Several key actions are needed to mitigate confusion around EBP and to help clinicians understand the differences between quality improvement, implementation science, EBP, and research.
Keywords: evidence-based decision making; evidence-based practice; healthcare; patient outcomes; patient safety; return on investment.
© 2023 The Authors. Worldviews on Evidence-based Nursing published by Wiley Periodicals LLC on behalf of Sigma Theta Tau International.
Publication types
- Systematic Review
- Delivery of Health Care*
- Evidence-Based Practice* / methods
- Quality Improvement
- Open access
- Published: 24 October 2024
Nurses’ implementation of evidence based practice in nursing process and its associated factors in South Wollo Zone public hospitals, Northeast Ethiopia: a mixed method study
- Afework Edmealem 1 ,
- Nurye Fentaw 2 ,
- Abebe Bekele 2 ,
- Belachew Tegegne 3 ,
- Jemal Mohammed 4 &
- Tiliksew Liknaw 1
BMC Nursing volume 23 , Article number: 782 ( 2024 ) Cite this article
1753 Accesses
Metrics details
Evidence-based practice is clinical decision-making using the best evidence available in the context of individual patients’ preferences and clinical expertise. It is serving as a crucial instrument for the health science disciplines to minimize the theory-practice gap although the level of practice is unknown. Thus, this study aimed to assess nurses’ implementation of evidence-based practice in nursing process and its associated factors in South Wollo Zone Public Hospitals.
An explanatory sequential mixed method was employed from April 1 to May 29, 2023, among 419 nurses for the quantitative part and 15 others for the qualitative part. The data were collected using structured, pretested, self-administered questionnaires. Simple random and purposive sampling techniques were used to select participants for the quantitative and qualitative studies, respectively. The bivariable analysis was done primarily, and variables with a p -value < 0.25 were further examined using a multivariable logistic regression model to control con-founders. Then, variables having a p -value less than 0.05 with a 95% CI were used to declare significantly associated factors. The key informants were interviewed using pre-made interview guidelines, and then open code software was utilized to conduct a thematic analysis.
Nurses who had poor implementation of evidence-based practice in the nursing process were 228 [54.42%; 95% CI: (49.8–59.3)]. Similarly, the key informants concluded that the implementation of evidence-based practice in the nursing process was low. Participants who were 31– 40 years old [AOR = 0.61, 95% CI: (0.38–0.99)], 41–50 years [AOR = 0.32, 95% CI: (0.15–0.65)], working at general hospitals [AOR = 3.37, 95% CI: (1.39–8.18)] and comprehensive specialized hospitals [AOR = 7.29, 95% CI: (3.06 − 17.31)], lack of training about evidence-based practice (AOR = 2.50, 95% CI: (1.36–4.56)], and lack of internet access [AOR = 2.46, 95% CI: (1.43–4.23)] were factors associated with poor levels of nurses’ implementation of evidence-based practice in the nursing process. The absence of computers, libraries, and updated guidelines were other factors identified on the quality analysis.
Nurses’ implementation of evidence-based practice in the nursing process was low. Age, working in general hospitals, and comprehensive and specialized hospitals, lack of training, and internet access were factors that had significant associations. Hence, hospital managers should give an attention to internet access and training about utilization of evidence-based practice in nursing process, particularly for those aged above thirty years old.
Peer Review reports
Introduction
Evidence-Based Practice (EBP) is a method of clinical practice in which clinicians use the most recent research and their clinical knowledge to arrive at recommendations for a given client while taking into account their preferences and values [ 1 , 2 ]. According to the International Council of Nurses, EBP is a tool used by the nursing discipline to reduce the theory-practice gap [ 3 ]. Its influence on nursing care dates back to Florence Nightingale in the first decade of the 19th century and grew between 1900 and 1970 with the founding of the American Nursing Association in 1920 and the first nursing research journal in 1952 [ 4 ].
Nowadays, EBP has become a crucial instrument of health care practice, and health professionals are expected to use the best evidence on a wide range of health science issues. It is stated that in order to improve procedures and close gaps, health practitioners should use evidence [ 3 ]. Improved patient outcomes, health service quality, patient safety, and clinical effectiveness, as well as improved professional performance, could exist with the integration of the best available research evidence, clinical expertise, patient values and preferences [ 5 , 6 ].
Nursing process is an organizing framework for professional nursing practice, which is a critical reasoning process to provide the best care to the client [ 7 ]. Efficient nursing process implementation improves care quality, speeds up the healing process, and reduces hospital stays while increasing patient satisfaction and service use [ 8 ]. It was believed that its implementation should be on the basis of updated guidelines and evidences [ 8 , 9 ].
Although EBP has been regarded as a crucial component to enhancing the quality of healthcare services and achieving excellence in patient care, EBP implementation in clinical settings has proven difficult in many countries due to different factors such as lack of time and lack of skills to find and manage research evidences [ 10 , 11 ]. Due to this, healthcare system administrators and other professionals have failed to ensure the ongoing performance improvement [ 12 ].
The proportion of nurses who had poor implementation of evidence-based practice was 58% in the nationwide survey in Taiwan [ 13 ]. It was found to be significantly low in sub-Saharan countries (54%) [ 14 ], including Ethiopia (47%) [ 15 ]. Another systematic review and meta-analysis done in Ethiopia reported that 57.06% of health care professionals had poor implementation of EBP [ 16 ]. Studies attempt to show significantly associated factors behind this low achievement. Problems at the individual level include a low level of knowledge, a lack of familiarity with EBP, an inability to synthesize the available literature, and resistance to change [ 17 , 18 , 19 ]. Organizational factors associated with poor level of implementation of EBP include lack of access to scientific literatures, computers, readily available research reports, and increased workload [ 20 , 21 , 22 ]. Educational status, work experience, marital status and favorable attitude were the other mentioned factors [ 15 , 23 ]. The nursing process enables nurses to perform their activities with scientific evidence and helps them to function as an autonomous and distinct profession; however, little is known about the implementation of the nursing process in accordance with EBP [ 24 ].
One of the most important frameworks for nurses is the nursing process. They can provide holistic care when they use the nursing process as a tool. Therefore, the implementation of EBP in the health care delivery system is essential, as it could improve the quality of care and patient safety [ 25 ]. However, there was a shortage of studies on the extent of EBP implementation with regard to the nursing process among nursing professionals in Ethiopia. Thus, this study aimed at bridging this gap and exploring factors.
Methods and materials
Study area and period.
The study was conducted in South Wollo Zone. There is one comprehensive specialized, four general, and nine primary hospitals. There are a total of 714 nurses who are working in these hospitals [ 26 ]. The study was conducted from April 1 to May 29, 2023.
Study design
An explanatory sequential mixed method was employed. First, the quantitative data were collected and analyzed. Then, to elaborate on the findings, particularly the associated factors, the qualitative data were collected and analyzed.
Source and study population
All nurses working at South Wollo Zone Public Hospitals were source population while those available at all hospitals during the data collection period were study population.
Inclusion and exclusion criteria
All nurses working in South Wollo Zone public hospitals and who are recruited permanently were included in this study. All nurses who were taking sick, annual and maternal leave were excluded.
Sample size determination
The sample size for the quantitative part was determined by using the single population proportion formula. According to a recent Ethiopian study, the proportion of nurses who had poor implementation of EBP was 45% [ 27 ]. The margin of error was 5% at a 95% confidence level. The sample size for the secondary objective was calculated by using sex, work experience, and the current position of nurses, and it was 213, 200, and 140, respectively.
N- sample size.
Z α/2- Level of confidence at 95%.
P = population proportion = 45%.
d- Margin of error = 5%.
After calculating the sample size for all objectives, the highest sample size was obtained from the first objective. By adding 10% non-response rate (38), the final sample size was 419. The sample size for the qualitative part was determined by saturation of ideas, and here, 15 key informants (5 from each level of institutions) participated in the interview.
Sampling technique and sampling procedure
The total sample size was allocated to each hospital proportionally based on the total number of nurses in each hospital. After that, samples from each hospital were again proportionally allocated to each working unit. Finally, participants were selected from each working unit by using simple random sampling using the list of nurses from the Human Resource Department (Fig. 1 ). Purposive sampling was used to select managers and department heads for key informant interviews.
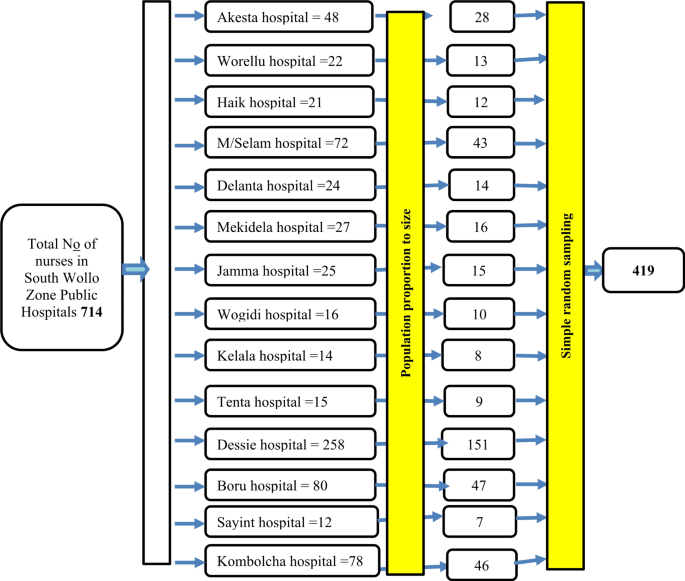
Schematic presentation of sampling technique in a study to assess implementation of EBP in nursing process and its associated factors among nurses working at South Wollo Zone Public Hospitals
Study variables
The dependent variable was nurses’ implementation of EBP in nursing process while the independent variables were sociodemographic characteristics (sex, age, educational status, and work experience, position, salary), knowledge of participants towards EBP, attitude of participants towards EBP, and presence of language difficulty, and organizational factors (training, internet access, and support from managers, working institution, working unit, availability of time to search evidences, having authority to change practice, presence of computer, and presence of library).
Data collection tool
A structured self-administered questionnaire prepared in English was used for quantitative data collection, and interview guides (Supplementary File 1 ) in Amharic were used for qualitative data collection with the help of audio recorders and a note book. This study assessed nurses’ implementation of evidence-based practice in nursing process using EBP implementation tool containing eighteen lists of activities. Frequency of each of activity for the last two months (8 week) had been assessed and responses labeled zero to four. The scales rated as 0 for those not implemented EBP at all, 1 for those implemented 1–3 times, 2 for those implemented 4–5 times, 3 for those implemented 6–7 times, and 4 for those implemented ≥ 8 times. After sum-up the value of each scale replied by participants, the maximum score was 66 and the minimum was 5 from the possible total score of 72. It was adapted from a study conducted in Iran with a validity of 0.96 and a reliability of 0.83 of Cronbach’s alpha value [ 28 ]. Similarly, the qualitative section has sociodemographic items and interview guides.
Operational definitions
Implementation EBP in nursing process tool have eighteen lists of items, each scaled from 0 to 4, then sum up for a possible minimum score of zero and a maximum of 72. The data was distributed normally as Skewness 0.38 and Shapiro Wilk, test found 0.34 so mean (40±11) was used to make cutoff point in to good and poor implementation status. Hence, participants who scored less than the mean (41) were considered as having ″poor implementation of EBP in nursing process. Respondents who scored below the mean (< 15.6) from the total knowledge score were categorized as having ″Inadequate knowledge about EBP in nursing process″. Furthermore, respondents who scored below or equal the mean (≤ 22) from attitude assessment questions were categorized as having ″unfavorable attitude towards implementation of EBP in nursing process″ [ 29 ]. Primary hospitals are referral centers for health centers and render general medical services like basic surgical, medical, maternal, and pediatric care to all patients, with approximately 25–50 beds. General Hospital are referral centers for primary hospitals and provide services such as general medicine, general surgery, obstetrics, gynecology, pediatric clinics along with few basic diagnostic and therapeutic services, with the capacity of 50 to 200 beds. Comprehensive Specialized Hospital care for patients who presented with variety of life discrepancies requiring complex and sophisticated attention, with greater than 200 beds and with all inhouse medical facilities [ 30 ].
Data collection procedure
Fourteen BSc nurses from health centers were trained as data collectors and two as supervisors. Questionnaires were distributed to participants with adequate time allocation, and supervisors followed the data collection process closely. A key informant interview was held in a safe and silent space with the help of audio recorders and a note book, and an average 20-minute probing time was employed in accordance with the participant’s response. Participants were allowed to express what they had to say openly without restriction concerning the issue.
Data quality control
The tool was pre-tested on 10% of nurses (38) at Kemissie Hospital for its appropriateness two weeks before the actual data collection. During data collection, the supervisors followed the day-to-day data collection process and ensured the completeness and consistency of the self-administered questionnaires each day before transferring them into computer software. Problems concerned with data collection were corrected early, and a non-overlapping numerical code was given for each question to enter in Epi-Data Manager version 4.6.
A silent place was chosen, high-quality audio recorders were used, and no book was used to describe exceptional events and emotions. Open-ended questions were forwarded for key informant interviews, and probing was done accordingly. The key informant’s interview was held without interruption, and additionally, issues that were not addressed were forwarded again by the principal investigator. In order to improve the data’s dependability, the initial data, codes, classifications, and topics were kept.
Data processing and analysis
After data collection, responses were checked and entered into a computer using the Epi Data Manager statistical package, and SPSS version 26 was used for data analysis. Descriptive statistics (frequencies and percentages) were calculated for all variables. Initially, assumptions were checked prior to the binary logistic regression analysis. The logistic regression analysis model was fit with a Hosmer and Lemeshow test of 0.89. Then, bivariable logistic regression analysis was carried out to see the association between the outcome and each explanatory variable. Sixteen variables with p -value less than 0.25 in bivariable logistic regression were exported to multivariable logistic regression analysis and a p -value < 0.05 was used to declare a statistical significance with respective crude and adjusted odds ratios.
For qualitative data, key informant interviews in the Amharic version of audiotape records were transcribed and translated to English, then entered into open code software for thematic analysis. The translation and transcription were done by the principal investigator after repeated listening based on Jeferson’ transcription code. Firstly, we went over the transcripts, listened to the recorded interviews, and then read them again to make sure we understood the information. Then, we categorized, classified, and highlighted all significant meaning units, text, and content linked to the study’s objectives. Since we were using open code software , we were free to make changes and additions to the codes at any time while they were being written. After analysis, the results were presented and triangulated to support the quantitative findings.
Socio-demographic characteristics of study participants
A total of 419 study participants were involved in this study, with response rate of 100%. Of all, two hundred thirty-six (56.3%) were females, while nearly four fifth (79%) were bachelor degree holders, and only 26(6.2%) were masters. Majority of participant’s (72.3%) were married, and 404 (96.4%) were working for 8 and less hours. The median working experience was 9 years. Regarding salary, more than half (51.3%) were paid 6501–9000 Ethiopian Birr (ETB) per month, and the median salary was 8017 ETB (Interquartile Range (IQR) -1985). (Table 1 )
Knowledge about EBP, language skill, and availability of time
Among all, 151 [36%, 95% CI: (31.4–40.6)] of them had inadequate knowledge about EBP in nursing process. Nearly two fifth (39.6%) had difficulty of interpreting literatures while two hundred eighty-four (67.8%) reported that they have no enough time to search evidences from different sources. (Table 2 )
Attitude towards EBP implementation in nursing process among nurses
Among all, 94 [22.4%, 95% CI: (18.4–26.4)] of them had unfavorable attitude towards implementation of EBP in nursing process. (Table 3 )
Organizational factors
Three hundred fifty-two (84%) of the participants didn’t take training about EBP in the nursing process, while nearly four fifth (79.5%) had no internet access. Two hundred fifty (59.7%) reported that they have no ability to influence the existing clinical practice. Similarly, two hundred sixty-one (62.3%) did not get support from their managers to implement EBP in the nursing process. Furthermore, nearly half (49.6%) reported that there were no guidelines for EBP in the nursing process. (Table 4 )
Nurses’ implementation of evidence-based practice in nursing process
According to the result, participants who had poor implementation of evidence-based practice in nursing process were 228 [54.42%, 95% CI: (49.8–59.3)]. (Fig. 2 )

Percentage of nurses’ implementation of EBP in nursing process in South Wollo Zone Public Hospitals, Northeast Ethiopia, 2024
Factors associated with nurses’ implementation of EBP in nursing process
Variables which had an association with implementation of EBP in nursing process at p value < 0.25 in bivariable logistic regression were age, level of institution, availability of internet access, training on EBP, and support from managers. All these variables were entered into multivariable logistic regression to identify factors. However, in multivariable logistic regression, only age, level of institution, internet access and taking training on EBP were associated with implementation of EBP in nursing process at P value of 0.05. Accordingly, 61% of nurses whose age was 31–40 years old were less likely to have poor implementation towards EBP in the nursing process [AOR = 0.61, 95% CI: (0.38–0.99)]. Furthermore, participants who were working at general, and comprehensive and specialized hospitals were 3.4 times [AOR = 3.37, 95% CI: (1.39–8.179)] and 7.3 times [AOR = 7.29, 95% CI: (3.07–17.31)] more likely to have poor implementation of EBP in the nursing process, respectively, compared to those working at primary hospitals. Similarly, participants who didn’t take training about EBP were 2.5 times more likely to have poor implementation of EBP in the nursing process [AOR = 2.50, 95% CI: (1.36–4.56)]. Moreover, nurses who didn’t have internet access were 2.5 times more likely to have poor implementation of EBP in the nursing process when compared to those who had internet access by any means [AOR = 2.46, 95% CI: (1.43–4.23)]. (Table 5 )

Qualitative findings
The qualitative data gained from 15 key informants. Of them, ten were males while eight of them were a master’s degree holder. Two of them were managers, and the rest 13 were supervisors (department heads). Moreover, twelve were working in inpatient departments. (Table 6 )
The open code analysis output showed that a number of codes with a variety of repetitions merged to form nine subthemes, and again, these subthemes merged to produce three main themes: level of implementation of EBP, factors affecting implementation of EBP, and opportunities to implement EBP. (Table 7 ).
Theme 1: nurses implementation of EBP in nursing process
The majority of key informants reported that implementation of EBP in nursing process is suboptimal.
“ As to my observation in the last 11 years , most of us including me are initiated to see the updated information such the nursing diagnosis terms from accessible sources. If one can not update him/her self , how can he/she implement EBP in nursing process or nursing care. In general speaking , nurses’ implementation of EBP in nursing process is very low. Nurses’ update themselves only when they are trained officially. ” ( A 36 years old head nurse ).
“The answer for the question for how much nurses implements EBP in nursing process is sub optimal because if nurses’ are trained well on the updated and new evidences , they can implement it. The problem is nurses are not able to update themselves and implement EBP in nursing process.” (28 years matron) .
Theme 2: factors associated with implementation of EBP in nursing process
Subtheme 1: sociodemographic characteristics.
Qualitative data support the quantitative finding, as the majority of key informants mentioned that younger nurses, those with masters and above, could exercise evidence-based practice in the nursing process.
Like , “I believe it is not well practiced in our hospital setup; nurses may also not be familiar with it except for masters and some other highly active professionals. What differentiates masters and youngsters in this regard , he said once more. Those who are older and more remote from recently updated internet-available scientific explanations are less active in using their handphones to access updated evidence than newly graduated nurses. They may not even own a smartphone and may not be comfortable with how to use one , which prevents them from using evidence-based nursing practices.” (38 years old head nurse) .
Subtheme 2: personal interest and skill related factors
The finding from qualitative analysis illustrated that knowledge and attitude of nurses towards EBP were among the determinant factors of implementation of EBP in the nursing process. The majority of the informants reported that low awareness of nurses about EBP, not updating oneself, lack of interest in using evidence among nurses, inability to understand scientific papers due to language barriers, misunderstanding of findings, and poor habit of reading were among the factors that were categorized under the subtheme personal interest and skill related factors. One replied for the question, "what are the factors affecting the implementation of EBP in the nursing process?" as
“Nurses are rarely encouraged to take advantage of opportunities to do it , and some are unaware of its relevance. I believe it has to do with our bad reading habits. Even many of us didn’t know where to look for scientific explanations and recommendations.” (37 years old head) .
Subtheme 3: organizational factors
The majority of key informants reported that the hospital environment is not convenient to exercise EBP. There is a lack of technologically advanced materials, organizations are not supportive of EBP, there is a lack of training about EBP, there is a lack of free internet access, and computers are among the factors affecting the implementation of evidence-based practice, which are under the subtheme organizational factors. Additionally, key informants probed to justify the relationship between nurses’ implementation of EBP in the nursing process and internet access. The majority of key informants replied that the current charge for internet access with mobile data is not affordable for many nurses.
“ I am aware of how expensive it is to utilize mobile data for any web access requirements. To be completely honest , it is currently impossible to even fully recharge a mobile phone for call service. Every department should have access to computers and the internet within the hospital’s compound.” (38 years old key informant) .
The majority of respondents explained the possible reasons behind many of the organizational problems, as the majority of key informants said financial constraints and the poor attention of higher officials regarding them were prior problems. One replied for the question, "what makes it difficult to avail resources that are important to implementing EBP?" as
“ I believe there should be funding for it , but instead , the budget was allocated mostly for medical expenses and other matters , and administrative bodies , including myself , paid it less attention.” ( Key informant 6 (matron) , whose age is 46 years old) .
Theme 3: opportunities of nurses to implement EBP in nursing process
Having a chance to work with expertise, going to other health care setting for experience sharing, meeting different individuals and attending seminars and workshops were the opportunities than enable nurses to implement EBP in nursing process.
“I tried to apply EBP while caring for my patients , particularly while using the nursing process as a framework. I gathered some updated information while reading articles during my thesis work for six months. I also got updated information during my postgraduate class. If I don’t have these opportunities , it is difficult to provide care with the updated information.” (Key informant 12 , whose age is 37) .
“As to me , nurses applied EBP in nursing process and other nursing services when someone told them the updated information in a certain circumstance. The main circumstance at which nurses update themselves is training. Nurses under my supervision are highly cooperative if they are told new information. ( Key informant 10 , whose age is 47) .
“Nurses who are working with senior physicians are more likely implement EBP since they got updated information while they working with them. Without having such opportunity , it is difficult for nurses to seek evidences and apply accordingly.” (Key informant 6 , whose age is 34) .
This study aimed at assessing nurses’ implementation of evidence-based practice in the nursing process and associated factors in South Wollo Zone hospitals. The current study revealed that 54.42% [95% CI: (49.8–59.3)] of nurses had poor implementation of evidence-based practice (EBP) in the nursing process, which was supported by qualitative findings as the majority of key informants reported that implementation of evidence-based practice in the nursing process among nurses was low in their institution.
The proportion of study participants who had poor implementation of EBP in this study is slightly higher than studies conducted in Ethiopia, 47% in north Gondar [ 31 ], 45.5% in West Arsi [ 32 ] and 48.2% at Jimma [ 33 ]. The possible justification for this might be the difference in the leadership, administration and socio demographic characteristics. Nurses are motivated and improve their commitment to their duty when there is a good leader [ 34 , 35 ].
On the other hand, the finding of this study is lower than those of the studies conducted in the Amhara region among nurses and midwives (65.2%) [ 36 ] and in Southwest Ethiopia among health care workers (63.8%) [ 37 ]. The variation might be due to differences in the study population, as in the current study conducted among nurses, the formers included other health care workers. The difference might be occurred since nurses have different knowledge and attitude towards EBP compared to others [ 38 ]. Furthermore, the result of this study is higher than the utilization level of health professionals in the study done in northwest Ethiopia [ 29 ]. The variation might be due to a difference in study population as it was conducted among health care workers at different institutional setups, which was only among nurses in the current study.
This study revealed that the odds of having poor implementation of EBP in the nursing process among nurses aged 31–40 years and 41–50 years were 61% and 32% less likely, respectively, when compared to that of nurses aged ≤ 30 years. This finding is supported by evidence that using updated evidence and technologies was declining as the age advanced and undoubtedly brought challenges for a generation born outside of the digitalized world prior to the internet age [ 39 ]. Unlikely, the majority of key informants replied that those who are old are fixed to old ways, and their participation in using currently available evidence and technologies in the nursing process is less likely.
Nurses who were working at general hospitals were 3.4 times more likely to have poor implementation of EBP in the nursing process, when compared to nurses who were working at primary hospitals. Similarly, nurses who were working at comprehensive specialized hospitals were 7.3 times more likely to have poor implementation of EBP in the nursing process, when compared to nurses who were working at primary hospitals. This may be due to the relatively high work load and patient flow in general and specialized hospitals [ 40 ]. Additionally, lack of support and mentoring, burnout and exhaustion, lack of continuing education, and fragmented nursing might be other reasons for the poor implementation in specialized and general hospitals [ 41 ].
Moreover, the odds of having poor implementation of EBP in the nursing process among nurses who didn’t take training were 2.5 times more likely compared with those who took training. It was mentioned by the majority of key informants as one of the problems related to the implementation of EBP in the nursing process. It was a determinant factor in a systematic review of low- and middle-income countries in Zambia [ 42 ] and Gondar [ 43 ]. The possible reason for this might be the poor trend of low- and middle-income countries to update nurses with refresher training [ 44 ].
Nurses who have no internet access were 2.5 times more likely to have poor implementation of EBP in the nursing process when compared to those with internet access by any means. In the same way, lack of free internet access was among the challenges for EBP in the nursing process mentioned by key informants. They reflected that the current charge for internet access with mobile data is not affordable for many nurses. Studies showed similar evidence in this regard [ 28 ]. Nowadays, guidelines, scientific evidence, and books are available online rather than in paper form. This makes internet access a crucial way to use them well.
Strength and limitation of the study
The study assessed factors using a mixed method design and focused on the implementation of EBP in a specific nursing clinical care, the nursing process. Moreover, the study was conducted in multiple healthcare settings.
Nurses’ implementation of EBP in the nursing process was low. Being 30 years of age and above; working at a general and comprehensive specialized hospital; lack of training about EBP; and internet access were among the variables that were significantly associated. The qualitative findings support the low nurses’ implementation of EBP in the nursing process and mentioned lack of internet access, the presence of computers, libraries, and updated guidelines as critical factors affecting the EBP in the nursing process. Hence, hospitals needed to have internet access to enhance access to updated medical evidences, particularly for those aged above thirty years old. In addition, the Ministry of Health, nursing professional associations, and partners should provide capacity building (such as training, mentorship, etc.) on EBP and infrastructures and resources (libraries, computers, and other digital devices) for nurses to utilize updated guidelines in each hospital. Moreover, we recommend quality offices within health facilities to support nursing managers in improving nursing care process utilization through different quality improvement projects and clinical audits.
Data availability
Data is provided within the manuscript.
Abbreviations
Adjusted Odds Ratio
Confidence Interval
Evidence Based Practice
Statistical Package for Social Sciences
Leen B, Bell M, McQuillan P. Evidence-based practice: a practice manual. 2014.
Melnyk BM, Fineout-Overholt E. Evidence-based practice in nursing & healthcare: a guide to best practice. Lippincott Williams & Wilkins; 2022.
Mackey A, Bassendowski S. The history of evidence-based practice in nursing education and practice. J Prof Nurs. 2017;33(1):51–5.
Article PubMed Google Scholar
Kim M, Mallory C, Valerio T. Statistics for evidence-based practice in nursing. Jones & Bartlett; 2020.
Yilak G et al. Implementation of nursing process and its associated factor among nurses at Woldia comprehensive specialized hospital, Northern Ethiopia: an institution-based cross-sectional study. Nursing: Res Reviews, 2022: pp. 111–9.
Stevens KR. The impact of evidence-based practice in nursing and the next big ideas. Online J Issues Nurs, 2013. 18(2).
Ackley BJ, et al. Nursing Diagnosis Handbook, Revised Reprint with 2021–2023 NANDA-I ® Updates-E-Book. Elsevier Health Sciences; 2021.
Sonğur C, et al. Patient safety culture, evidence-based practice and performance in nursing. Systemic Pract Action Res. 2018;31:359–74.
Article Google Scholar
Yates C. Evidence-based practice: the components, history, and process. Couns Outcome Res Evaluation. 2013;4(1):41–54.
Portney LG. Foundations of clinical research: applications to evidence-based practice. FA Davis; 2020.
Dalheim A, et al. Factors influencing the development of evidence-based practice among nurses: a self-report survey. BMC Health Serv Res. 2012;12:1–10.
Christenbery T, et al. Immersion in evidence-based practice fellowship program: a transforming experience for staff nurses. J Nurses Prof Dev. 2016;32(1):15.
Article PubMed PubMed Central Google Scholar
Hung H-Y, et al. Current state of evidence-based practice education for undergraduate nursing students in Taiwan: a questionnaire study. Nurse Educ Today. 2015;35(12):1262–7.
Boltena MT, et al. Adherence to evidence-based implementation of antimicrobial treatment guidelines among prescribers in sub-saharan Africa: a systematic review and meta-analysis. J Pharm Policy Pract. 2023;16(1):137.
Wudu MA, et al. Uptake of evidence-based practice and its predictors among nurses in Ethiopia: a systematic review and meta-analysis. Front Pharmacol. 2024;15:1421690.
Wubante SM, Tegegne MD. Evidence-based practice and its associated factors among health professionals in Ethiopia: systematic review and meta-analysis. Inf Med Unlocked. 2022;32:101012.
Hellier S. Factors affecting implementation of evidence-based practice among nurse practitioners. Indiana University of Pennsylvania; 2015.
Barako TD. Factors influencing application of evidence based practice (EBP) among nurses working in Kenyatta National Hospital (KNH)-Nairobi. 2011.
Aarons GA, et al. The organizational social context of mental health services and clinician attitudes toward evidence-based practice: a United States national study. Implement Sci. 2012;7:1–15.
Shewangizaw Z, Mersha A. Determinants towards implementation of nursing process. Am J Nurs Sci. 2015;4(3):45–9.
Pitsillidou M, et al. Factors affecting the application and implementation of evidence-based practice in nursing. Acta Informatica Med. 2021;29(4):281.
Kennedy M, et al. Factors affecting implementation of evidence-based practices in public health preparedness and response. J Public Health Manage Practice: JPHMP. 2020;26(5):434.
Zewdie A, et al. Determinants of evidence-based practice among health care professionals in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2023;18(11):e0293902.
Article CAS PubMed PubMed Central Google Scholar
Betty J, Ackley A, Ladwig S. Nursing diagnosis handbook: an evidence based guide to planning care. St Louis, Missouri: Mosby; 2011.
Google Scholar
Melnyk BM, et al. A study of chief nurse executives indicates low prioritization of evidence-based practice and shortcomings in hospital performance metrics across the United States. Worldviews Evidence‐Based Nurs. 2016;13(1):6–14.
Dessie Comprehensive Sepecialized Hospital. Human Resource Planning, 2023.
Degu AB, et al. Evidence-based practice and its associated factors among point-of-care nurses working at the teaching and specialized hospitals of Northwest Ethiopia: a concurrent study. PLoS ONE. 2022;17(5):e0267347.
Kalavani K, Mohebbifar R, Rafiei S. Evidence based practice among healthcare providers: a cross-sectional study. Int J Health Care Qual Assur. 2019;32(5):867–78.
Dessie G, et al. Evidence-based practice and Associated factors among Health Care providers Working in Public hospitals in Northwest Ethiopia during 2017. Curr Therapeutic Res. 2020;93:100613.
Ababa A. Federal Democratic Republic of Ethiopia ministry of health. Ethiopia: Postnatal Care; 2003.
Beshir MA, Woreta SA, Kebede M. Evidence-based practice among health professionals in hospitals of Northwest Ethiopia: a cross-sectional study. JBI Evid Implement. 2017;15(4):161–70.
Golge AM, et al. Implementation of evidence-based practice and its correlates among nurses working in southern Ethiopia. Int J Afr Nurs Sci. 2024;20:100691.
Hoyiso D, Arega A, Markos T. Evidence based nursing practice and associated factors among nurses working in Jimma Zone public hospitals, Southwest Ethiopia. Int J Nurs Midwifery. 2018;10(5):47–53.
Sfantou DF et al. Importance of leadership style towards quality of care measures in healthcare settings: a systematic review. in Healthcare. 2017. MDPI.
Fransen K, et al. When is a leader considered as a good leader? Perceived impact on teammates’ confidence and social acceptance as key ingredients. Int J Psychol Res. 2018;12:1–21.
Dagne AH, et al. Implementation of evidence-based practice and associated factors among nurses and midwives working in Amhara Region government hospitals: a cross-sectional study. Reproductive Health. 2021;18:1–10.
Shibabaw AA, et al. Evidence-based practice and its Associated factors among Health professionals Working at Public Hospitals in Southwest Ethiopia. Biomed Res Int. 2023;2023(1):4083442.
Weng YH, et al. Implementation of evidence-based practice across medical, nursing, pharmacological and allied healthcare professionals: a questionnaire survey in nationwide hospital settings. Implement Sci. 2013;8:112.
Birkland JL. How older adult information and communication technology users are impacted by aging stereotypes: a multigenerational perspective. New Media Soc. 2024;26(7):3967–88.
Hadgu G, et al. Assessment of nurses’ perceptions and barriers on evidence based practice in Tikur Anbessa specialized hospital Addis Ababa Ethiopia. Am J Nurs Sci. 2015;4(3):73–83.
Sist L, et al. The reasons for unfinished nursing care during the COVID-19 pandemic: an integrative review. Nurs Rep. 2024;14(2):753–66.
Lupenga J, et al. Evaluating evidence based practice of physiotherapists and the Quality of Physiotherapy Services in Selected Health Facilities of Lusaka, Zambia. Indonesian J Disabil Stud. 2019;6(2):133–42.
Bashar FJ. Assessing attitudes towards knowledge and use of evidence-based practice among nurses working in a Teaching Hospital in Kuala Lumpur. Int J Educ Lit Stud. 2019;7(1):25–30.
O’Donovan J, et al. Ongoing training of community health workers in low-income and middle-income countries: a systematic scoping review of the literature. BMJ open. 2018;8(4):e021467.
Download references
Acknowledgements
We, the authors, want to sincerely thank data collectors and study participants for their commitment. Additionally, we want to forward our deepest gratitude to South Wollo Zone Public Hospitals administrators for their strong support.
There is no fund for conducting the study.
Author information
Authors and affiliations.
Department of Nursing, Debre Markos University, Debre Markos, Ethiopia
Afework Edmealem & Tiliksew Liknaw
Tropical College of Medicine Dessie Campus and Dessie Comprehensive Specialized Hospital, Dessie, Ethiopia
Nurye Fentaw & Abebe Bekele
Department of Nursing, Injibara University, Injibara, Ethiopia
Belachew Tegegne
Department of Nursing, Wollo University, Dessie, Ethiopia
Jemal Mohammed
You can also search for this author in PubMed Google Scholar
Contributions
NF and AB conceived, designed, and collect the data. AE performed analysis, interpretation of data, advised and supervised the design conception. BT and TL drafted the manuscript. All authors read and approved the final Manuscript.
Corresponding author
Correspondence to Afework Edmealem .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was written with reference number TCOM/Res/1217/2015 on February 5, 2023, from the Tropical College of Medicine ERC (Ethical Review Committee). Permission was obtained from each hospital administrator after explaining the purpose and all the processes to set the appropriate data collection time by considering workload. All methods were carried out in accordance with relevant guidelines and regulations. Each participant gave their informed consent before taking part in the research. The individual participant had not been subjected to any harm as far as confidentiality is concerned.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Edmealem, A., Fentaw, N., Bekele, A. et al. Nurses’ implementation of evidence based practice in nursing process and its associated factors in South Wollo Zone public hospitals, Northeast Ethiopia: a mixed method study. BMC Nurs 23 , 782 (2024). https://doi.org/10.1186/s12912-024-02444-4
Download citation
Received : 05 February 2024
Accepted : 14 October 2024
Published : 24 October 2024
DOI : https://doi.org/10.1186/s12912-024-02444-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Evidence-based practice
- Nursing process
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Most Read Articles
15 December 2023
20 June 2024
20 September 2024
28 March 2024
- Toggle navigation About
Evidence Based Practice in Nursing: Evidence Based Articles
- Evidence Based Practice
Finding Articles
Apa citations.
- Glossary & Tutorials
- Critical Appraisal
InterLibrary Loan Service
If we don't have it, don't worry! Our InterLibrary Loan Service can help. We can borrow books and journal articles from another library.
Specialized databases are listed below. They will provide access to practice guidelines, systematic reviews, research articles, and other information related to evidence-based practice.
Comprehensive source for nursing and allied health journals. Provides full text for more than 1,300 journals. Coverage dates back to 1937. Includes searchable Cited References, Evidence-based Care Sheets, Continuing Education Modules Modules, and full text Research Instrument Records. EBSCO
Provides authoritative medical information on medicine, nursing, dentistry, veterinary medicine, the health care system, pre-clinical sciences, and much more. Created by the National Library of Medicine, MEDLINE allows users to search abstracts from over 4,000 current biomedical journals. MEDLINE Complete provides full text coverage for over 2,500 journals with more than 1,400 not found in other EBSCO full text databases. EBSCO
- Clinicaltrials.gov ClinicalTrials.gov is a registry and results database of federally and privately supported clinical trials conducted in the United States and around the world. ClinicalTrials.gov gives you information about a trial's purpose, who may participate, locations, and phone numbers for more details. This information should be used in conjunction with advice from health care professionals.
- Agency for Healthcare Research & Quality Evidence Reports The Agency for Healthcare Research and Quality (AHRQ), through its EPCs, sponsors the development of various reports to assist public- and private-sector organizations in their efforts to improve the quality of health care in the United States.
- TRIP Database Trip is a clinical search engine designed to allow users to quickly and easily find and use high-quality research evidence to support their practice and/or care.
National Library of Medicine PubMed is a database of over 15 million citations for articles published in more than 4800 biomedical journals and magazines from the U.S. and 70 other countries. Coverage dates back to the 1950's. Links to full text and related resources are included.
Full-text of important nursing journals not found in other databases - American Journal of Nursing; CIN: Computers, Informatics, Nursing; JONA's Healthcare Law, Ethics, and Regulation; JONA: The Journal of Nursing Administration; MCN, The American Journal of Maternal/Child Nursing; Nurse Educator; The Nurse Practitioner, Nursing 0X; and, Nursing Research. OVID
- DSM-5 Library This link opens in a new window Database contains the full content of: * DSM-5-TR * DSM-5 Handbook on the Cultural Formulation Interview * DSM-5 Handbook of Differential Diagnosis * DSM-5-TR Clinical Cases * Spanish Edition of the Desk Reference to the Diagnostic Criteria from the DSM-5 The library does not have access to legacy content. APPI
You will be required to cite your sources in American Psychological Association (APA).
Our citation guide has an APA Style tab, which includes resources that will be helpful in creating APA citations.
- Cite Your Sources by Tom Schilb Last Updated Oct 1, 2024 2100 views this year
- << Previous: Evidence Based Practice
- Next: Books >>

IMAGES
COMMENTS
Evidence-Based Nursing systematically searches a wide range of international healthcare journals applying strict criteria for the validity of research and relevance to best nursing practice. Content is critically appraised and the most relevant articles are summarised into succinct expert commentaries, focusing on the papers` key findings and ...
Nov 20, 2023 · Systems - integration of evidence with patient records Summaries - practice guidelines found via Clinical Key & UpToDate Synopses of Syntheses - focused journals: Evidence-Based Nursing, Evidence-Based Medicine, ACP Journal Club Syntheses - meta-analyses, systematic reviews and other evidence syntheses found through Cochrane, CINAHL, PubMed
Background: Evidence-based practice and decision-making have been consistently linked to improved quality of care, patient safety, and many positive clinical outcomes in isolated reports throughout the literature. However, a comprehensive summary and review of the extent and type of evidence-based practices (EBPs) and their associated outcomes ...
Oct 24, 2024 · Background Evidence-based practice is clinical decision-making using the best evidence available in the context of individual patients’ preferences and clinical expertise. It is serving as a crucial instrument for the health science disciplines to minimize the theory-practice gap although the level of practice is unknown. Thus, this study aimed to assess nurses’ implementation of evidence ...
Feb 8, 2023 · EBP experts at the Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare have recently published a dissemination guide that addresses all the key elements of EBP methodology (Dean et al., 2021) that could serve this purpose. Linking evidence to action
This collection of articles is from the Arizona State University College of Nursing and Health Innovation's Center for the Advancement of Evidence-Based Practice. Evidence-based practice (EBP) is a problem-solving approach to the delivery of health care that integrates the best evidence from studies and patient care data with clinician ...
Apr 23, 2024 · Florence Nightingale was the first nurse to use evidence to change practice, 2 and today, EBP continues to be an expectation of all nurses, including NPs. Although EBP has been integrated into nursing culture, less is understood about QI, perhaps because QI has its roots in industry and has been historically focused on sustained process improvement rather than clinical competency.
Dec 15, 2023 · Discover the most frequently read articles from the past month of Evidence-Based Nursing that have been published in the last 12 months.
Dec 16, 2024 · They will provide access to practice guidelines, systematic reviews, research articles, and other information related to evidence-based practice. CINAHL Complete This link opens in a new window Comprehensive source for nursing and allied health journals.
Recognition of the research-to-practice gap was described in 2000 by Balas and colleagues, who published a landmark paper in which they noted it takes an average of 17 years to translate a scientific discovery (such as an evidence-based recommendation) into real-world clinical practice and settings. 4 Since this gap was made transparent, an ...