- Open access
- Published: 10 March 2021

Measuring health inequalities: a systematic review of widely used indicators and topics
- Sergi Albert-Ballestar 1 , 2 &
- Anna García-Altés ORCID: orcid.org/0000-0003-3889-5375 1 , 2 , 3
International Journal for Equity in Health volume 20 , Article number: 73 ( 2021 ) Cite this article
19k Accesses
17 Citations
36 Altmetric
Metrics details
According to many conceptual frameworks, the first step in the monitoring cycle of health inequalities is the selection of relevant topics and indicators. However, some difficulties may arise during this selection process due to a high variety of contextual factors that may influence this step. In order to help accomplish this task successfully, a comprehensive review of the most common topics and indicators for measuring and monitoring health inequalities in countries/regions with similar socioeconomic and political status as Catalonia was performed.
We describe the processes and criteria used for selecting health indicators from reports, studies, and databases focusing on health inequalities. We also describe how they were grouped into well-known health topics. The topics were filtered and ranked by the number of indicators they accounted for.
We found 691 indicators used in the study of health inequalities. The indicators were grouped into 120 topics, 34 of which were selected for having five indicators or more. Most commonly found topics in the list include “Life expectancy”, “Infant mortality”, “Obesity and overweight (BMI)”, “Mortality rate”, “Regular smokers/tobacco consumption”, “Self-perceived health”, “Unemployment”, “Mental well-being”, “Cardiovascular disease/hypertension”, “Socioeconomic status (SES)/material deprivation”.
Conclusions
A wide variety of indicators and topics for the study of health inequalities exist across different countries and organisations, although there are some clear commonalities. Reviewing the use of health indicators is a key step to know the current state of the study of health inequalities and may show how to lead the way in understanding how to overcome them.
Introduction
Strong efforts to tackle health inequalities can be seen at international and national level since the 1980s. In early 2008, the World Health Organization’s (WHO) Global Commission on Social Determinants of Health called for action on the social determinants of health, the conditions in which persons are born, grow, work, live, and age, to “close the gap in a generation” [ 1 ]. In late 2008, the Spanish Public Health General Direction ( Dirección General de Salud Pública) and the Foreign Health of Health Ministry and Social Policy ( Sanidad Exterior del Ministerio de Sanidad y Política Social ) requested the constitution of the Commission for the Reduction of Social and Health Inequalities ( Comisión para Reducir las Desigualdades Sociales en Salud en España (CRDSS-E) [ 2 ]. The mission of CRDSS-E was to elaborate on a proposal of intervention measures to reduce health inequalities. The CRDSS-E published two documents: one analysing health inequalities in the Spanish context [ 3 ], and another describing some policy proposals to tackle them [ 4 ]. In 2011, a total of 125 countries, Spain being one of them, developed and signed the Rio Political Declaration on Social Determinants of Health [ 5 ]. The declaration recommended interventions from governments and international organisations [ 6 ].
At a regional level in Catalonia, tackling health inequalities is one of the main goals of both the Catalan Health Plan 2016–2020 (led by the Health Department of the Catalan Government) [ 7 ] and the Interdepartmental and Intersectorial Public Health Plan 2017–2020 (PINSAP) [ 8 , 9 ]. During the past years, various reports and peer-reviewed papers about the health effects of the economic crisis on the population of Catalonia were published by the Catalan Health System Observatory [ 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ].
Overall, much effort has been devoted to monitoring and tackling health inequalities at regional, national, and international levels. Even so, OECD countries continue to present large disparities in health, including, for example, significant differences in life expectancy between people with the highest and lowest levels of education [ 18 ]. The selection of topics represents the first step in monitoring health inequalities according to many conceptual frameworks and is highly relevant, as these topics will potentially limit the detection of health inequalities within the population, hence playing a key role in providing evidence for posterior decision-making [ 19 , 20 ]. Yet some difficulties may arise during the selection of relevant topics, as well as their health indicators. A wide diversity of indicators for monitoring health inequalities have been used across different countries and organisations; this is due to the high variety of contextual factors that may have an influence on it, such as the study goals or the information resources available.
In order to help accomplish this task successfully, the objective of this study is to perform a systematic review of the most common topics and indicators used for measuring and monitoring health inequalities in the reports, projects, and databases of international, national, and regional governmental organizations.
The main purpose of this study is to provide a broad overview of health inequalities topics considered relevant by different public health organizations. Nevertheless, the focus of this review is on countries/regions with similar socioeconomic and political status to Catalonia. It may also be useful for other organizations who decide to study or monitor health inequalities to accomplish its very first step: topic selection. In addition, gaining some insights about which health issues are being prioritized, as well as which indicators were used, are considered secondary goals.
Material and methods
First, a bibliographic search was performed using PubMed, Google Scholar, and Google search engine with the terms “ health inequalities ”, “ health observatories ” and “ health inequalities indicators ”. Occasionally, names of concrete regions, countries, or organisations were added to these terms (i.e., “ Andalucía health observatory ” or “ Canada health inequalities ”). The search was performed from March to June of 2019. Once finished, a set of inclusion criteria was applied; studies included in the review had to:
Include health inequalities indicators : All the reports that contained no health indicators were automatically discarded (i.e., policy frameworks [ 21 ]).
Have been carried out by a governmental organisation or a related entity, whether at an international, national, or regional level : the reports not published by governmental (or government-related) organisations were discarded.
Have a socioeconomic and political status similar (or highly related) to Catalonia : some reports were discarded due to significant differences in the socioeconomic profile of the countries they were studying in comparison to Catalonia or Spain.
Once the reports were selected, the authors performed a quality control check of the indicators shown in the reports and databases. The indicators had to match the basic anatomy of an indicator as a minimum requirement to be considered an indicator. This basic anatomy consists of containing data, i.e. the numerical data input; and containing good metadata, like a title and an explanation of how an indicator is defined and calculated [ 22 ]. In addition, the different reports found were classified according to the geo-political region they were studying: 1. international, 2. national, and 3. regional (Table 1 ).
After this selection process, the indicators were grouped into topics by semantic matching of their definition as well as by the area of knowledge there are intended to measure. Most of the topics were supported by references of relevant organisations like the WHO or the United Nations (UN) (see Table 2 ). Each topic was uniquely named in accordance with the area of knowledge that instruments were intended to measure. Indicators from different sources were often merged due to high similarities between them (most commonly, the only differences were stratifiers such as age, gender or region). Every topic had to be formed by at least five indicators in order to be considered relevant enough; the topics with less than five indicators were discarded.
The search was performed by the two researchers, and the results shared in order to agree on any discrepancies. All the data was organised in spreadsheets to identify common indicators, and then sorted by the amount of indicators they included. The names of the indicators in the spreadsheets were those given in the original reports or their metadata information.
In total, 21 reports, projects, and databases were identified and classified into three categories: 1. international [ 8 ], 2. national [ 10 ], and 3. regional [ 3 ]. In the first category, international, all the projects selected were carried out or funded by the European Commission [ 23 , 24 , 25 , 26 , 27 ], the WHO [ 28 , 29 ] or the World Bank [ 30 ]. In the following category, national, studies were conducted by health agencies or governments of countries such as Andorra [ 31 ], Australia [ 32 ], Canada [ 33 , 34 ], England [ 35 , 36 ], Scotland [ 37 ], Slovenia [ 38 ], Spain [ 39 ] or Portugal [ 40 ]. In the last category, regional, some reports published by Spanish regions were included (Andalucía [ 41 ], Barcelona [ 42 ], Valencia [ 43 ]). A total of 691 health indicators were identified (Table 1 ).
Following an iterative process of evaluation, we identified a core set of 120 candidate topics, of which 34 were finally selected (Fig. 1 ). Table 2 describes a complete list of 34 topics with the corresponding definition of each topic. The ten most commonly used were: “Life expectancy”, “Infant mortality”, “Obesity and overweight (BMI)”, “Mortality rate”, “Regular smokers/tobacco consumption”, “Self-perceived health”, “Unemployment”, “Mental well-being”, “Cardiovascular disease/hypertension”, “Socioeconomic status (SES)/material deprivation”. However, some topics that ranked below these were closely related with some of the most common topics; for example, “Perinatal, neonatal and stillbirths mortality” might be considered as a subtype of “Infant mortality”; and “Perceived mental health” is similar to both “Mental well-being” and “Self-perceived health”. Furthermore, some indicators may represent antithetically the same area of knowledge; that is the case for the indicators in the topic “Long-term limitations/chronic illnesses” and the indicator “Healthy Life Years (HLY)” [within the topic “Life expectancy”], where the former (long-term limitations or chronic illnesses) is used to determine the latter (the end of a healthy life condition). Nevertheless, the metadata of the health indicators within each topic was highly homogeneous: they all had similar definitions and methodology.
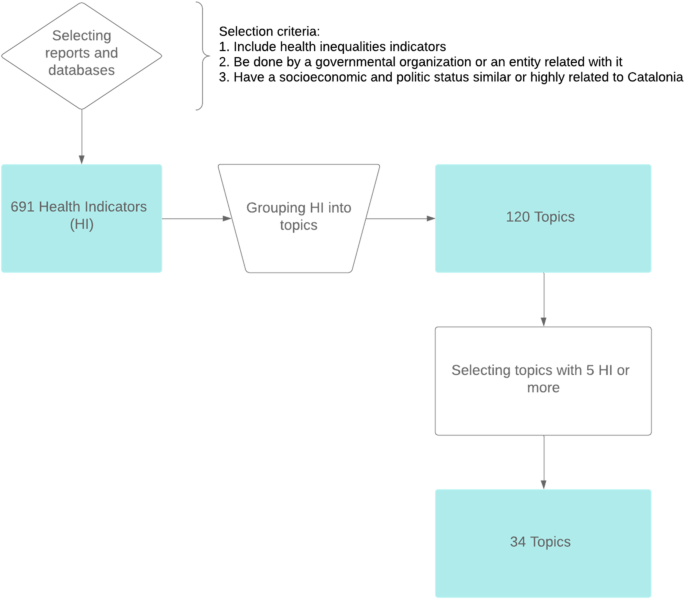
Flowchart of the processes undertaken to review the most common topics in the study of health inequalities
In general, the indicators within each topic were very similar. In fact, often the differences among them were related to the different stratifiers (such as sex, age or region) used for their calculation. For example, in the first topic “Life expectancy”, indicators have different variations: “Life expectancy at birth” [ 23 , 24 , 25 , 27 , 28 , 29 , 32 , 33 , 37 , 40 , 41 , 42 ], “Life expectancy at birth by sex” [ 22 , 24 , 25 , 26 , 27 , 33 , 34 ], “Life expectancy at a certain age” [ 25 , 33 , 35 , 40 ], “Life expectancy by educational attainment level” [ 25 ], and “Life expectancy at birth by socioeconomic status” [ 25 ]. Complex measures of inequality, such as “Slope index of inequality (SII) for male and female life expectancy” [ 34 ] may be considered another (more advanced) variation.
Furthermore, in the case of a health outcomes or diagnostics (such as mortality or cancer) the concrete disease or cause may also play an important role in the heterogeneity found among the health indicators. Indicators are focused on different aspects, such as prevalence and incidence, mortality, preventive measures, or treatments. For example, for the topic “HIV”: “HIV incidence” [ 23 , 26 , 28 , 33 , 40 ], “Prevalence of HIV, male/female, by ages” [ 29 , 39 ] and “AIDS-related mortality rate” [ 28 , 39 ] are the most common, yet “Antiretroviral therapy (ART) coverage” [ 28 ] and “HIV test results for TB patients (positive results)” [ 28 ] can also be relevant.
The results of the study show that the most common topics are related to:
Mortality/life expectancy: “Life expectancy” [ 44 , 45 ], “Infant mortality” [ 46 ] or “Mortality rate” [ 47 ] are widely used to study health inequalities.
Incidence/mortality rates of specific diseases: “Cardiovascular disease/hypertension”, “Cancer (incidence or mortality)” [ 48 ], “Diabetes/insulin resistance” [ 49 ], “HIV” [ 50 ], “Tuberculosis (TB)” [ 51 ] or “Respiratory diseases”.
Social determinants of health [ 52 ]:
◦ “Living and working conditions” where this could be studied at an individual level, was highly ranked: “Unemployment” [ 53 ] and “Primary studies/illiteracy”. Otherwise, these indicators were at the bottom of the list.
◦ This was similar for “Individual lifestyle factors and social and community networks” topics, which can also be studied at an individual level: “Obesity and overweight (BMI)” [ 54 , 55 ], “Regular smokers/tobacco consumption” [ 56 ], “Alcohol consumption” [ 57 ], “Hazardous alcohol consumption”, “Physical activity” [ 58 ], and “Food consumption (vegetables, fruit, salt)”.
◦ Socioeconomic level: “Socioeconomic status (SES)/material deprivation” [ 59 , 60 ].
◦ Healthcare system: “Healthcare resources” and “Policy and Legislation”.
Main results of the study
The results of the study showed that the most common topics were related to mortality/life expectancy, incidence/mortality rates of specific diseases (i.e., TB or HIV), and social determinants of health, such as living and working conditions, and individual lifestyle factors and social and community networks, according to Dahlgren and Whitehead’s model of the social determinants of health [ 52 ]. The indicators that can be studied at an individual level tended to be highly ranked, in comparison to those that are studied at different levels (such as hospital or region), which tended to be at the bottom. Many methodological differences between indicators were due to stratifiers in their calculation.
Study selection criteria
To include health inequalities indicators was a fundamental requirement for any report in order to be included in the review. Hence, although some reports provided in-depth insights about tackling health inequalities (i.e., [ 21 , 61 ]) they were not selected due to lack of health indicators monitoring.
In addition, to be carried out by a governmental or a government-related organisation was also an important requirement, as many academic and/or private institutions carry out studies and reviews of health inequalities, but their policy-making influence is limited. Their reports tend to be focused on concrete knowledge fields, such as gender influence [ 62 ], the effects of economic crises [ 63 ], or access to healthcare [ 64 ]; which are also relevant for the study of health inequalities but whose authorship does not fit the selection criteria, as the main interest of this paper is identifying the health inequalities indicators used by health agencies or similar government-related entities. The reports not produced by this kind of organisation were rejected.
Lastly, to have a socioeconomic and politic status similar or highly related to Catalonia criteria was intended to exclude reports whose health indicators were adapted to least developed/developing countries where, for example, access to treatments of diarrhea for infants may still be an issue [ 65 ]. Hence, some reports were discarded due to significant differences in the socioeconomic profile of the countries they are studying in comparison to Catalonia or Spain.
These criteria were applied to all the reports and studies found after an extensive search. The addition of country/region names in the search responded to the need of knowing how particular regions of interest were dealing with health inequalities. Interest in regions was mainly based on previous knowledge of concrete public health organizations studying those regions, as well as interest in looking for other organizations in charge of tackling health inequalities in regions similar to Catalonia. Nevertheless, as in any review, it is not possible to ensure that absolutely all the reports suitable for this study were found during the search, nor that they were selected after applying the selection criteria.
Grouping health indicators into topics
As stated above, the most frequent health indicators were grouped into topics according to the health domain they were measuring (with each indicator related to only one topic). For example, although “ Percentage of 15-year-olds who were overweight in 2009–10, EU Member States by sex ” [ 25 ] and “ Obesity rate by body mass index (BMI) (sdg_02_10) ” [ 23 , 66 ] are different indicators per se, they are both intended to measure the same health issue and, hence, were grouped under the same topic “Obesity and overweight (BMI)” under the indicator name “Obesity and/or overweight (total, by sex, age, or educational level)”.
Most of the selected health indicators were taken from the official statistics of different countries or international organisations, whose development and methodology has been closely consolidated over many years and respond to international standards. In addition, most of these indicators are related to relevant knowledge areas for the study of health inequalities, such as lifestyle habits, deprivation, and mortality .
To prioritise the most relevant topics, all the groups with less than five health indicators were deleted. This meant that, unfortunately, interesting topics such as the “Years of potential life lost” [ 34 , 36 , 42 ], “Unmet health needs” [ 23 , 26 , 39 ] and “Passive smokers” [ 33 , 34 ] were not taken into consideration. Nevertheless, this selection does not imply per se a periodic monitoring of the selected health indicators, as specific topics not present in this list may be studied according to ultimate needs.
Relevance of the most common topics
All the topics aim to measure and study the relation between determinants of health and health outcomes. Interestingly, three of the top five topics in the list (see Table 2 ) are related to mortality: life expectancy, infant mortality, and mortality rate. Life expectancy at birth is an indicator of mortality conditions and, by proxy, of health conditions [ 44 ]. Hence, life expectancy as well as other mortality-related topics are widely used in the study of health inequalities.
Living and working conditions, such as BMI or smoking, are also key factors in the study of health inequalities as both share a strong socioeconomic gradient [ 54 , 56 ]. Therefore, as may be expected, they appeared among the top 10 positions in the list of topics (see Table 2 ). According to our review, the most common way to measure socioeconomic status is to analyse the unemployment rates and material deprivation level of the population.
In Spain, some regions use less common health indicators for studying health inequalities that may be interesting for particular knowledge areas. For example, the Valencian Observatory of Health uses the “Caregiver profile”, which they report to be mostly women, without primary studies, 57-years-old on average, and reporting bad self-perceived health. In addition, they also use “Reasons why contraceptive methods are not used by age and nationality of women” as well as a “Sexual-health information resources (school, parents, friends, etc.)”, which may help to understand possible sexual health inequalities [ 43 ]. In the Andalusian School of Public Health, the indicator “Psychosis and mental illnesses due to drugs or alcohol abuse” may be helpful to estimate various negative health outcomes of alcohol and substance abuse that the healthcare system will need to address [ 41 ]. Even so, more than a half of topics in Table 2 appear in their reports.
As may be expected, the health indicators used in other reports produced by the Catalan Health System Observatory, such as the “Community Health Indicators”, match the implicit measurement concept behind many of the topics: obesity and overweight, mortality by age (including infant), self-perceived health, and population with primary studies are some of them [ 67 ].
- Health indicators
As can be seen in Table 3 , health indicators were combined within each topic if stratifiers such as population sex, age, or region were the only difference in their calculation methodologies. Some indicators were also merged if they were formerly different in the way they expressed the same data (i.e., raw number, rate per 1000 or 100,000).
The health indicators within each topic often cover a different aspect relevant to health inequalities. For example, in the topic “Tuberculosis” [ 23 , 29 , 33 , 34 , 40 , 42 , 43 ] indicators about incidence, prevalence, or mortality can be observed. In addition, health indicators about treatment coverage or vaccination are also included in this topic. Overall, in most topics, indicators try to measure every relevant (and measurable) aspect of the topic.
Common stratifiers are sex, age, and studied region, something that is coherent with the determinants of health perspective and the focus on inequalities. However, the stratifiers found are highly heterogeneous and may also include socioeconomic status, educational level, or nationality/country of origin, among many others.
Research fitted to monitor health inequalities
This comprehensive review was carried out to help accomplish the first step in the process for tackling and monitoring health inequalities: selecting high-impact issues and health indicators [ 19 , 20 ]. The next steps in the analysis will be to carefully take into account stratifiers such as area of residence, gender, age, and nationality. Lastly, after the identification of key health inequalities, decision-making stakeholders will need to play a role during the last steps: determining priorities of action and implementing changes. The time variable will play a key role in the monitoring, as it will indicate the possible health consequences of policy-making decisions [ 19 , 20 ].
Reviewing the most common health indicators and topics used in the study of health inequalities may help research teams in different ways. First, having an overview of what is being done by their neighbouring countries or regions may highlight issues that should not be missed when selecting relevant health topics to study. Second, even if some topics might not ultimately be chosen as a priority of action, having a complete list of key issues will provide an overview of what is relevant in the study of health inequalities, as well as some interesting insights. Lastly, knowing what other research institutions are working on will promote potential collaborations between organizations, creating synergies and bonds that may lead to better understanding and monitoring of health inequalities.
At a regional level, these results are highly valuable for the first stages of health inequalities monitoring cycles in Catalonia. This study provided the basis for choosing health topics to study as well as helped gain insights about which indicators should be used. In addition, regions with similar socioeconomic status and goals in tackling health inequalities may benefit from this research. Similarly, at a national and international level these results may help organizations shift the focus towards undermined health inequalities topics or explore new areas of knowledge (yet unstudied or with a different perspective).
Availability of data and materials
No analysis of quantitative data was performed. Hence, data availability declaration is not applicable.
Abbreviations
Acquired immune deficiency syndrome
Acute myocardial infarction
Bacillus Calmette-Guérin
Body mass index
Chronic obstructive pulmonary disease
Comisión para Reducir las Desigualdades Sociales en Salud en España
Cardiovascular disease
European Core Health Indicators
12-Item General Health Questionnaire
General practitioner
Human Immunodeficiency Virus
Healthy Life Years
International Classification of Diseases, Clinical Modification
International Health Regulations
National Health Service
Portable document format
Public Health Agency of Canada
Interdepartmental and Intersectorial Public Health Plan
Percutaneous transluminal coronary angioplasty
Sustainable Development Goals
Socioeconomic status
Slope index of inequality
Tuberculosis
Uniform resource locator
United Nations
World Health Organization
World health organization (WHO). Meeting report of the world conference on social determinants of health. Rio de Janeiro, 19-21. Geneva: WHO; 2011. p. 2012. http://www.who.int/sdhconference/resources/wcsdh_report/en/ . Accessed 24 July 2019
Google Scholar
Comisión para Reducir las Desigualdades Sociales en Salud en España. Propuesta de políticas e intervenciones para reducir las desigualdades sociales en salud en España. Gac Sanit. 2012:182–9.
Comisión para Reducir las Desigualdades Sociales en Salud en España. Análisis de situación para la elaboración de una propuesta de políticas e intervenciones para reducir las desigualdades sociales en salud en España. Madrid: Ministerio de Sanidad y Política Social; 2009. http://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/promocion/desigualdadSalud/docs/Analisis_reducir_desigualdes.pdf . Accessed 24 July 2019.
Comisión para Reducir las Desigualdades Sociales en Salud en España. Avanzando hacia la equidad: propuesta de políticas e intervenciones para reducir las desigualdades sociales en salud en España. Madrid: Ministerio de Sanidad y Política Social; 2010. http://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/promocion/desigualdadSalud/docs/Propuesta_Politicas_Reducir_Desigualdades.pdf . Accessed 24 July 2019.
World Health Organization (WHO). Rio political declaration on social determinants of health Rio de Janeiro, Brazil. Geneva: WHO; 2011. p. 2012. https://www.who.int/sdhconference/declaration/en/ . Accessed 24 July 2019
Working Group for Monitoring Action on the Social Determinants of Health. Towards a global monitoring system for implementing the Rio Political Declaration on Social Determinants of Health: developing a core set of indicators for government action on the social determinants of health to improve health equity. Int J Equity Health. 2018;17(1):136.
Article Google Scholar
Government of Catalonia. Health plan for Catalonia 2016–2020. Barcelona: Ministry of Health of Catalonia; 2016. http://salutweb.gencat.cat/web/.content/_departament/pla-de-salut/Pla-de-salut-2016-2020/documents/health-plan-catalonia_2016_2020.pdf . Accessed 24 July 2019
Comissió Interdepartamental de Salut. Pla interdepartamental i intersectorial de salut pública. Barcelona: Ministry of Health of Catalonia; 2017. http://salutpublica.gencat.cat/web/.content/minisite/aspcat/sobre_lagencia/pinsap/01Els_Plans/PINSAP_2017-2020/PINSAP_2017-2020-Complet.pdf . Accessed 24 July 2019
Cabezas-Peña C. Catalonia, Spain. Regions for Health Network (RHN). Geneva: WHO; 2018. http://www.euro.who.int/__data/assets/pdf_file/0004/373387/rhn-catalonia-eng.pdf . Accessed 24 July 2019
Observatori del Sistema Salut de Catalunya. Efectes de la crisi econòmica en la salut de la població de Catalunya. Barcelona: Agency for Health Quality and Assessment of Catalonia; 2014. http://observatorisalut.gencat.cat/web/.content/minisite/observatorisalut/contingutsadministratius/observatori_efectes_crisi_salut_document.pdf . Accessed 24 July 2019
Observatori del Sistema Salut de Catalunya. Efectes de la crisi econòmica en la salut de la població de Catalunya. Anàlisi territorial. Agency for Health Quality and Assessment of Catalonia: Barcelona; 2015. http://observatorisalut.gencat.cat/web/.content/minisite/observatorisalut/ossc_crisi_salut/Fitxers_crisi/Salut_crisi_informe_2015.pdf . Accessed 24 July 2019
Observatori del Sistema Salut de Catalunya. Desigualtats socioeconòmiques en la salut i la utilització de serveis sanitaris públics en la població de Catalunya. Agency for Health Quality and Assessment of Catalonia: Barcelona; 2017. http://observatorisalut.gencat.cat/web/.content/minisite/observatorisalut/ossc_crisi_salut/Fitxers_crisi/Salut_crisi_informe_2016.pdf . Accessed: 13 September 2019
Observatori del Sistema Salut de Catalunya. Central de Resultats: Efectes de la crisi econòmica en la població infantil de Catalunya. Barcelona: Agency for Health Quality and Assessment of Catalonia; 2014. http://observatorisalut.gencat.cat/web/.content/minisite/observatorisalut/contingutsadministratius/observatori_efectes_crisi_salut_monografic.pdf . Accessed 20 March 2020
Observatori del Sistema Salut de Catalunya. Central de Resultats: Evolució de la utilització de serveis i el consum de fàrmacs 2008–2015. Barcelona: Agency for Health Quality and Assessment of Catalonia; 2008. http://observatorisalut.gencat.cat/web/.content/minisite/observatorisalut/ossc_central_resultats/informes/fitxers_estatics/MONOGRAFIC_25_CRISI_EVOLUCIO_2008-2015.pdf . Accessed 20 Mar 2020
García-Altés A, Ruiz-Muñoz D, Colls C, Mias M, Martín BN. Socioeconomic inequalities in health and the use of healthcare services in Catalonia: analysis of the individual data of 7.5 million residents. J Epidemiol Community Health. 2018;72(10):871–9.
Article PubMed PubMed Central Google Scholar
Ruiz-Muñoz D, Colls C, Mias M, Martín N, García-Altés A. Desigualtats socioeconòmiques en la salut i la utilització dels serveis sanitaris públics en la població de Catalunya. Ann Med. 2017;100:172–6 https://www.academia.cat/files/499-448-FITXER/provesievidencies1.pdf . Accessed 20 Mar 2020.
Genoveva B, Ruiz-Muñoz D, García-Altés A. Efectes de la crisi econòmica en la salut de la població de Catalunya: anàlisi territorial. Ann Med. 2016;99:126–31 https://www.academia.cat/files/499-386-FITXER/provesievidencies.pdf . Accessed 24 July 2019.
Health for Everyone?. OECD Health Policy Studies. Paris: OECD; 2019. https://www.oecd-ilibrary.org/social-issues-migration-health/health-for-everyone_3c8385d0-en . Accessed 9 Jan 2021.
World Health Organization (WHO). Handbook on health inequality monitoring with a special focus on low- and middle-income countries. Geneva: WHO; 2013.
UK Department of Health. Health equity audit: a self-assessment tool. London: Department of Health, 2004: 25. https://webarchive.nationalarchives.gov.uk/20120105214155/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4070715 . Accessed 13 Sept 2019.
WHO Regional Office for Europe. Health 2020: A European policy framework and strategy for the 21st century. Geneva: WHO; 2013:190. http:// www.euro.who.int/__data/assets/pdf_file/0011/199532/Health2020-Long.pdf . Accessed 24 July 2019.
Pencheon D. The good indicators guide: understanding how to use and choose indicators. Coventry: NHS Institute for Innovation and Improvement; 2017. https://www.england.nhs.uk/improvement-hub/publication/the-good-indicators-guide-understanding-how-to-use-and-choose-indicators . Accessed 25 Mar 2020
Eurostat. SDG 3. Good health and well-being. Luxembourg: European Commission. https://ec.europa.eu/eurostat/web/sdi/good-health-and-well-being . Accessed 8 Apr 2020.
ECHI-European Core Health Indicators. Luxembourg: European Commission. https://ec.europa.eu/health/indicators/echi/list_en#id3 . Accessed 8 Apr 2020.
Marmot M. Health inequalities in the EU - final report of a consortium. Luxembourg: Publications Office of the European Union; 2013. [ https://ec.europa.eu/health//sites/health/files/social_determinants/docs/healthinequalitiesineu_2013_en.pdf ]. Accessed 8 Apr 2020
Social Protection Committee. Indicators Sub-group. Portfolio of EU social indicators for the monitoring of progress towards the EU objectives for social protection and social Inclusion. Luxembourg: Publications Office of the European Union; 2015. http://ec.europa.eu/social/BlobServlet?docId=14239&langId=en . Accessed 8 Apr 2020
I2sare project. Galicia, Spain profile. Regional Health Profiles in the European Union, 2010. www.sergas.es/Saude-publica/-I2SARE-Galicia . Accessed 8 Apr 2020.
World Health Organization (WHO). Data Management Tool. Copenhagen: WHO Regional Office for Europe. http://dmt.euro.who.int/classifications/tree/B#B02 . Accessed 8 Apr 2020.
World Health Organization (WHO). 100 core health indicators (plus health-related SDGs). Geneva: WHO; 2018. www.who.int/healthinfo/indicators/100CoreHealthIndicators_2018_infogr.April 2020. Accessed 8 April 2020
The World Bank. Health. Data. Washington DC: The World Bank. https://data.worldbank.org/topic/health . Accessed 8 Apr 2020.
Observatori Social d'Andorra. Sant Julià de Lòria (Andorra): Centre d’Estudis Andorrans. Govern d'Andorra https://observatorisocial.ad/index.php . Accessed 8 Apr 2020.
Turrell G, Stanley L, de Looper M. Oldenburg B. Health inequalities in Australia: morbidity, health behaviours, risk factors and health services use (AIHW). Canberra; 2006. www.aihw.gov.au/getmedia/0cbc6c45-b97a-44f7-ad1f-2517a1f0378c/hiamhbrfhsu.pdf . Accessed 8 Apr 2020
Public Health Agency of Canada. Key Health Inequalities in Canada: A National Portrait. Ottawa: Government of Canada; 2018. http://www.canada.ca/en/public-health/services/publications/science-research-data/key-health-inequalities-canada-national-portrait-executive-summary.html . Accessed 8 Apr 2020
Canadian Institute of Health Information. Health Inequalities Data Tool. Ottawa: Government of Canada https://health-infobase.canada.ca/health-inequalities/data-tool/index . Accessed 8 Apr 2020.
Institute of Health Equity. Marmot indicators release 2017. London: Institute of Health Equity; 2017. http://www.instituteofhealthequity.org/about-our-work/marmot-indicators-release-2017 . Accessed 8 Apr 2020
NHS England Analytical Services & the Equality and Health Inequalities Unit. England Analysis: NHS Outcome Framework Health Inequalities Indicators. London: NHS England; 2016. http://www.england.nhs.uk/wp-content/uploads/2017/07/nhs-outcome-framework-health-inequalities-indicators-2016-17.pdf . Accessed 8 Apr 2020
Scottish Government. Long-term monitoring of health inequalities. Scottish Government: Edinburgh; 2018. http://www.gov.scot/publications/long-term-monitoring-health-inequalities-december-2018-report . Accessed 8 Apr 2020
Buzeti T, Djomba JK, Blenkuš MG, Ivanuša M, Klanšček HJ, Kelšin N, et al. Health inequalities in Slovenia. Ljubljana: National Institute of Public Health; 2011. http://www.euro.who.int/__data/assets/pdf_file/0008/131759/Health_inequalities_in_Slovenia.pdf . Accessed 8 Apr 2020
Ministry of Health and Social Policy of Spain. Moving forward equity in health: monitoring social determinants of health and the reduction of health inequalities. Madrid: Ministry of Health and Social Policy of Spain; 2010. http://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/promocion/desigualdadSalud/PresidenciaUE_2010/conferenciaExpertos/docs/haciaLaEquidadEnSalud_en.pdf . Accessed 8 Apr 2020
Instituto Nacional de Estatística-Statistics Portugal. Indicadores Sociais 2011. Lisbon: Instituto Nacional de Estatística-Statistics Portugal; 2012. https://censos.ine.pt . Accessed 8 Apr 2020
García-Calvente MM, del Río LM, Marcos-Marcos J. Guía de indicadores para medir las desigualdades de género en salud y sus determinantes. Escuela Andaluza de Salud Pública. Junta de Andalucía: Granada; 2015. http://www.easp.es/project/guia-de-indicadores-para-medir-las-desigualdades-de-genero-en-salud-y-sus-determinantes . Accessed 8 Apr 2020
Malmusi D. Desigualtats en salut, respostes a nivell local: Polítiques per reduir les desigualtats en salut a la ciutat de Barcelona. Barcelona: Ajuntament de Barcelona; 2017. http://www.consorci.org/media/upload/arxius/coneixement/salut-publica/2017/D_%20Malmusi_Desigualtats_28-09-2017.pdf . Accessed 8 Apr 2020
Observatorio Valenciano de la Salud. Desigualdades en Salud en la Comunidad Valenciana. Valencia: Generalitat. Conselleria de Sanitat Universal i Salut Pública; 2018. http://www.sp.san.gva.es/DgspPortal/docs/20180301_Desigualdades_Salud_OVS2018.pdf . Accessed 8 Apr 2020
United Natios (UN). Life expectancy at birth. New York: UN. http://www.un.org/esa/sustdev/natlinfo/indicators/methodology_sheets/health/life_expectancy.pdf . Accessed 19 Mar 2020.
Shryock HS, Siegel JS, Stockwell EG. The methods and materials of demography. San Diego: Academic Press; 1976.
Global Health Observatory (GHO) data. Infant mortality. Geneva: World Health Organization (WHO); 2018. http://www.who.int/gho/child_health/mortality/neonatal_infant/en/ . Accessed 8 Apr 2020
Porta M, editor. A dictionary of epidemiology, sixth edition. Oxford: Oxford University Press; 2016. http://www.oxfordreference.com/view/10.1093/acref/9780199976720.001.0001/acref-9780199976720 . Accessed 8 Apr 2020
World Health Organization (WHO). Cancer. Geneva: WHO. http://www.who.int/health-topics/cancer#tab=tab_1 . Accessed 7 Apr 2020.
World Health Organization (WHO). Diabetes. Geneva: WHO. http://www.who.int/health-topics/diabetes#tab=tab_1 . Accessed 7 Apr 2020.
World Health Organization (WHO). HIV/AIDS. Geneva: WHO. http://www.who.int/health-topics/hiv-aids#tab=tab_1 . Accessed 7 Apr 2020.
World Health Organization (WHO). Tuberculosis. Geneva: WHO. http://www.who.int/health-topics/tuberculosis#tab=tab_1 . Accessed 7 Apr 2020.
Bambra C, Gibson M, Sowden A, Wright K, Whitehead M, Petticrew M. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J Epidemiol Community Health. 2010;64(4):284–91.
Article CAS PubMed PubMed Central Google Scholar
Organisation for Economic Co-operation and Development (OECD). OECD Glossary of Statistical Terms-Unemployed–ILO Definition. Paris: OECD; 2003. https://stats.oecd.org/glossary/detail.asp? ID=2791. Accessed 7 Apr 2020
Pigeyre M, Rousseaux J, Trouiller P, Dumont J, Goumidi L, Bonte D, et al. How obesity relates to socio-economic status: identification of eating behavior mediators. Int J Obes. 2016;40(11):1794–801.
Article CAS Google Scholar
World Health Organization (WHO). Obesity and overweight. Geneva: WHO. http://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight . Accessed 7 Apr 2020
WHO, Tobacco and inequities Guidance for addressing inequities in tobacco-related harm Written by: Belinda Loring. 2014.
World Health Organization (WHO). Harmful use of alcohol. Geneva: WHO. http://www.who.int/health-topics/alcohol#tab=tab_1 . Accessed 7 Apr 2020.
World Health Organization (WHO). Physical activity. Geneva: WHO. http://www.who.int/news-room/fact-sheets/detail/physical-activity . Accessed 7 Apr 2020.
American Psychological Association (APA). Socioeconomic Status. Washinton DC. http://www.apa.org/topics/socioeconomic-status/ . Accessed 6 Apr 2020.
Eurostat. Glossary: Material deprivation - Statistics Explained. Luxembourg: European Commission. https://ec.europa.eu/eurostat/statistics-explained/index.php/Glossary:Material_deprivation . Accessed 6 Apr 2020.
Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2. Geneva: World Health Organization (WHO); 2010. p. 79.
Salcedo N, Saez M, Bragulat B, Saurina C. Does the effect of gender modify the relationship between deprivation and mortality? BMC Public Health. 2012;12:574.
Regidor E, Barrio G, Bravo MJ, de la Fuente L. Has health in Spain been declining since the economic crisis? J Epidemiol Community Health. 2014;68(3):280–2.
Article PubMed Google Scholar
Consulting Services Limited ICF. Towards a fairer and more effective measurement of access to healthcare across the EU final. London: ICF; 2018. https://ec.europa.eu/health/sites/health/files/cross_border_care/docs/2018_measurement_accesstohealthcare_frep_en.pdf . Accessed 6 Apr 2020
Ebinger JO, Hamso B, Gerner F, Lim A, Plecas A. Europe and Central Asia region. New York: World Bank; 2008. https://elibrary.worldbank.org/doi/abs/10.1596/25984 . Accessed 6 Apr 2020
Book Google Scholar
Eurostat. Eurostat - Tables, Graphs and Maps Interface (TGM) table. Luxembourg: European Commission; 2018. https://ec.europa.eu/eurostat/tgm/table.do?tab=table&init=1&language=en&pcode=sdg_02_10&plugin=1 . Accessed 28 Feb 2020
Catalan Healthcare System Observatory. Indicadors de salut comunitària. Barcelona: Agència de Qualitat i Avaluació Sanitàries de Catalunya. Departament de Salut; 2017. http://observatorisalut.gencat.cat/ca/observatori-desigualtats-salut/indicadors_comunitaria/ . Accessed 25 Mar 2020
Download references
Acknowledgements
We thank Neus Carrilero-Carrió (Agència de Qualitat i Avaluació Sanitàries de Catalunya (AQuAS), Barcelona, Spain) for support in reviewing drafts and assistance with writing.
All the activities performed were funded by the Agència de Qualitat i Avaluació Sanitàries de Catalunya (AQuAS) and CIBER de Epidemiología y Salud Pública (CIBERESP).
Author information
Authors and affiliations.
Catalan Health System Observatory, Agència de Qualitat i Avaluació Sanitàries de Catalunya (AQuAS), 81-95 (2a planta), 08005, Barcelona, Spain
Sergi Albert-Ballestar & Anna García-Altés
CIBER de Epidemiología y Salud Pública (CIBERESP), Barcelona, Spain
Institut d’Investigació Biomèdica (IIB Sant Pau), Barcelona, Spain
Anna García-Altés
You can also search for this author in PubMed Google Scholar
Contributions
SA performed the main bibliographic review as well as the selection and organisation of health indicators and topics. AGA supervised the whole process, contributed to the conceptualisation of the paper and provided extensive comments and improvements to the drafts. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Anna García-Altés .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Albert-Ballestar, S., García-Altés, A. Measuring health inequalities: a systematic review of widely used indicators and topics. Int J Equity Health 20 , 73 (2021). https://doi.org/10.1186/s12939-021-01397-3
Download citation
Received : 06 October 2020
Accepted : 28 January 2021
Published : 10 March 2021
DOI : https://doi.org/10.1186/s12939-021-01397-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health inequalities
- Health policy
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Transforming health systems to reduce health inequalities
Sarah sowden, jasmine olivera, clare bambra, alex gimson, rob aldridge, carol brayne.
- Author information
- Copyright and License information
Address for correspondence: Dr John Ford, Forvie Site, University of Cambridge School of Clinical Medicine, Cambridge Biomedical Campus, Cambridge CB2 0SR, UK. Email: [email protected] Twitter: @johnford1849
Never before in history have we had the data to track such a rapid increase in inequalities. With changes imminent in healthcare and public health organisational landscape in England and health inequalities high on the policy agenda, we have an opportunity to redouble efforts to reduce inequalities.
In this article, we argue that health inequalities need re-framing to encompass the breadth of disadvantage and difference between healthcare and health outcome inequalities. Second, there needs to be a focus on long-term organisational change to ensure equity is considered in all decisions. Third, actions need to prioritise the fundamental redistribution of resources, funding, workforce, services and power.
Reducing inequalities can involve unpopular and difficult decisions. Physicians have a particular role in society and can support evidenced-based change across practice and the system at large. If we do not act now, then when?
KEYWORDS: health inequalities, equity, health systems, healthcare organisations
Introduction
For the first time in history we have the empirical data to witness a rapid compounding of existing inequalities due to the COVID-19 pandemic, particularly for lower socio-economic and minority ethnic groups. 1,2 In the UK, deaths in the most deprived areas are double those in the least deprived (age–sex standardised rate in the least deprived areas are 350 deaths per 100,000 compared with 669 in the most). 3 In the USA and UK, deaths are up to three times higher in minority ethnic groups. 4 The current crisis represents a syndemic pandemic; the intertwined, interactive and cumulative effects on health and wellbeing of the COVID-19 pandemic combined with substantial existing socio-economic inequalities across life courses and in communities. 2
Despite the policy prominence and various frameworks focusing on health inequalities, healthcare leaders still do not feel they have the skills and knowledge to reduce health inequalities. 5–9 The underlying reasons for this may include a failure of researchers to provide accessible evidence on how to translate evidence into practice as well as a lack of a systematic and logical approach to inequalities for healthcare systems. 10–12 Physicians have a particular role in society and can support evidence-based change across practice and the system at large. Here, we first discuss the current policy and research context, then argue it is time for a re-framing of inequalities within healthcare systems, with a concerted effort to build a long-term organisational change to tackle inequalities head on, along with a wider redistribution of resources, funding, workforce, services and power across healthcare and wider society.
Policy, research and legislative context of health systems in the UK
In England, for the first time, key national and local NHS decision-making bodies were required by law to address inequalities in access and outcomes under the Health and Social Care Act 2012. 13 This was the result of a growing body of literature showing sustained stark health outcome inequalities, dating back to the Black report, with inequalities in waiting times, patient experience and hospital admissions. 14–17 The Health and Social Care Act also shifted power from ministerial departments to NHS England with a decentralisation of decision making to local health systems. Despite the statutory responsibility, the years after the enactment of the Health and Social Care Act were dominated by reorganisation with considerable fragmentation of previously aligned services. Reforms were undertaken in the name of efficiency with poor evidence of their impact, rising costs to the health system and little progress on health inequalities, despite the clear negative health and wellbeing impacts of austerity and welfare reform. 18,19 Public health professionals classified the risk of this reorganisation to widen health inequalities as ‘extreme’. 20
In 2019, the NHS in England was asked to develop its own plans for a £20 billion funding injection. High-level policy objectives and initiatives were outlined in The NHS Long Term Plan and, in turn, local healthcare systems were asked to develop their own local response plans. 21 Health inequalities were a prominent feature of the national The NHS Long Term Plan among other priorities, such as primary care workforce, integration, prevention, cardiovascular disease and cancer. The plan set out to establish a ‘more concerted and systematic approach to reducing health inequalities’ alongside a number of specific inequalities initiatives such as supporting minority ethnic groups. However, the plan and its subsequent supporting documents failed to outline how local and national systems could systematically approach health inequalities with an expectation that local healthcare systems would each develop their own approaches. Our own previous research has highlighted that this is challenging for local systems, resulting in local plans being vague and lacking a systematic or joined-up approach. 12 Furthermore, the lack of a national health inequalities strategy (like that successfully pursued between 2000 and 2010) makes it harder to effect change across local health systems. 22,23
In response to COVID-19 inequalities data, NHS England and NHS Improvement (NHSE/I) published eight urgent actions to address health inequalities, including directives protecting the most vulnerable, improving recording, strengthening leadership and increasing preventative measures. 24
The structure of the NHS has moved substantially from its inception, through many re-disorganisations and, lately, the statutory bodies established under the Health and Social Care Act 2012. More recently, integrated care systems have been established, which are likely to merge with clinical commissioning groups. 25 It is likely that further health and social care legislation, under the advice of NHSE/I, will be passed in the near future to catch up with the organisational evolution. 26
Only 7 years after its formation, Public Health England (PHE) is already being disestablished. PHE was set up to protect and improve the nation's health and reduce health inequalities. 27 One action of the Health and Social Care Act was the extraction of public health skills from leadership roles within the NHS, something that was an obvious gap immediately after revealing a lack of understanding of the key role of public health leadership and skills in health and social care systems. This has become critical during the COVID-19 pandemic, as more public health leadership in the health and social care system may have improved the response.
Health inequalities have been a common thread across PHE activities. While trying work across organisational boundaries, these have included the provision of data on health inequalities, guidance, evidence-based tools for local health systems, advice to national government and focused action on inequalities in screening and immunisations. 5 , 28–31 PHE have particularly promoted a place-based approach to inequalities. 5 Under current plans PHE's health protection functions will be taken over by the National Institute for Health Protection, but the future location of the other PHE functions is still under discussion.
The research community has been driving forward the inequalities' agenda. The Academy of Medical Sciences published their report Improving the health of the public by 2040 promoting a health of the public research approach with a strong emphasis on health equity. 32 In response to this, the Strategic Coordination of the Health of the Public Research committee (SCHOPR) was established and has set out its guiding principles on population research, including a priority of focused investigation into how interdisciplinary research can reduce inequalities. 33 Furthermore, the Academy of Medical Sciences has recently written to the secretary of state outlining the need to prioritise prevention and improvement to reduce inequalities. 34
More recently, the Royal College of Physicians have convened a coalition of over 140 organisations to campaign for a cross-government strategy to reduce inequalities, the commencement of the socio-economic duty in the Equality Act and prioritising child health in public policy. 35
With the healthcare and public health reform afoot, inequalities highlighted due to the pandemic are thus high on the policy agenda, and a mobilised research community, it is time to rethink our approach to inequalities within and beyond the healthcare system. Without clarity, sufficient prioritisation and leadership any actions are at risk of only ever having a marginal impact.
Framing inequalities to ensure a systematic and logical approach in health systems
Framing is a way of structuring or presenting a problem and can be helpful, potentially vitally so, to ensuring action. 36 How we discuss and present inequalities must be developed with and for any audience it is hoped might contribute to effective changes; for example, NHS staff are more likely to engage if inequalities are framed around healthcare and the specific services for which they are responsible, such as inequalities in chronic disease management or non-elective admissions alongside concrete actions, rather than high-level more abstract health outcome inequalities, such as differences in life expectancy. 37 A lack of adequate framing brings risks. Focusing only on high level inequalities with healthcare staff, such as life expectancy, may lead to a sense of fatalism because these inequalities are primarily driven by geo-political factors outwith the influence of local health systems and their leaders; or a belief that downstream individual actions targeted at the social determinants of health will reduce inequalities. 38–40 In turn, these may lead to a health inequalities fatigue where motivation for action on inequalities wains due to short-termism and a perceived lack of progress.
A broad framing of inequalities highlighting how multiple different aspects of disadvantage lead to substantial differences in healthcare and health outcomes is needed to allow decision-makers to develop their own systematic and logical approach to doing what is within their power and advocacy to reduce inequalities. Without this systematic approach, there is a risk of an unequal focus on certain groups at the expense of others, such as focusing on the so-called ‘deserving poor’ at the expense of the ‘undeserving poor’. 41 Our review of local NHS plans revealed that systems focused more on people with learning difficulties and autism, but less so on undocumented migrants, people who are transgender or those with justice service involvement. 12 This creates inequalities within inequalities.
Inequalities must be framed and measured to include both healthcare (eg risk factor management, access, diagnosis, treatment and experience) and health outcome (eg morbidity and mortality) inequalities (Fig 1 ). Key components across the spectrum of health and care include the distribution of health system resources (namely funding, workforce and research distribution, and training), access to and quality of healthcare, major drivers of mortality and morbidity (eg cardiovascular disease, respiratory disease, cancer, mental health and musculoskeletal conditions) and conditions which are intrinsically associated with inequalities (such as drug and alcohol abuse).
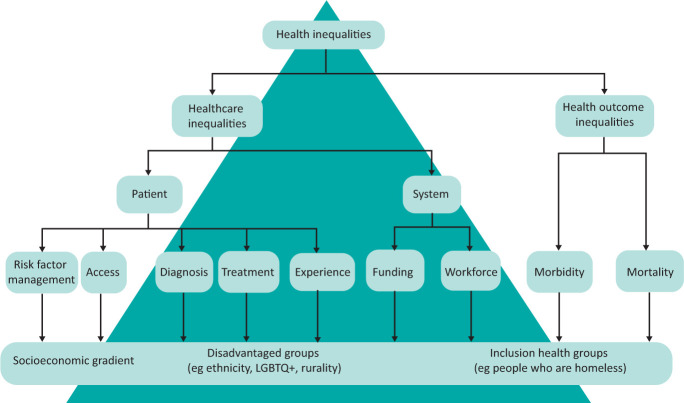
Unpacking health inequalities.
Framing should avoid language which is stigmatising or shaming. Smith and colleagues describe a paradox where people recognise that health is determined by social factors and acknowledged socio-economic inequalities in society, but are reluctant to acknowledge the resulting health inequalities. 42 The authors suggest this paradox arises because individuals do not want the place in which they live to be stigmatised, shamed, or have negative or derogatory connotations, which may have negative impacts on their employment opportunities or family. 43 Other studies have found that the idea of socio-economic health inequalities can be a source of stress for residents. 44,45
Building the long-term organisational change
Many health inequalities have arisen over decades and even centuries, operating across generations and communities, due to long-standing imbalances in the social determinants of health. It is noteworthy that the north-south pattern of deaths from the Spanish flu pandemic of 1918, almost exactly mirrors the distributions of COVID-19 deaths over a century later. 46 New manifestations of inequalities emerge over time, often with the promise of solutions and enthusiasms from new technologies. Previously this was the offer of screening, known to be taken up preferentially by more advantaged in society, and more recently in access to digital healthcare services with clear differential access. 47 In light of the plethora of existing and emerging inequalities, many feel a moral duty to ‘do something’, including investments in actions that lack a strong evidence base or sustainability (such as social prescribing or hospitals acting as anchor institutions). 48 It is important, therefore, for the NHS to resist the temptation to reach for such short-term actions at the expense of focusing on the long-term organisational change required for sustained and evidenced-based action. With the formation of integrated care systems in the NHS in England we have the opportunity to ensure an equity perspective is adopted from the start, maximising the opportunities of integrated working across health and social care. However, we need inequalities actions at all levels of healthcare, including national, system, organisational and individual (Fig 2 ).
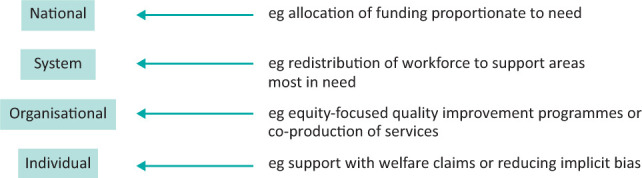
Levels of health inequalities actions.
Much health data, particularly within hospitals, is not presented by socio-economic group, geographical disadvantage or ethnicity. The NHS eight urgent actions to address inequalities aims to improve ethnicity recording. 24 More upskilling is needed to help healthcare analysts undertake equity analyses to explore the difference between groups, adjusting for age and gender where appropriate. Equity perspectives are still rarely considered in healthcare quality improvement programmes, clinical audits, service evaluation or adverse events investigation; for example, hospital-based quality improvement programmes should consider if the services changes improve quality of care across socio-economic groups and ethnicity equally. Adverse event investigations should include an exploration how healthcare supported (or not) patients who are disadvantaged, for example due to poor health literacy or social support, interacted with services.
Previous research suggests that equity-focused processes can support healthcare organisations, their teams and individuals within these to address inequalities. 49 Health inequalities impact assessment is a process of exploring and mitigating the impacts of decisions on inequalities during decision making. Sadare and colleagues found that health inequalities impact assessment, if undertaken a meaningful way, can be a catalyst for equity-focused organisational change. 49 These could be used by clinical directors and hospital leaders to ensure that secondary care services do not increase inequalities.
Applied research has an vital role to play in exploring the distributional effects of interventions across disadvantaged groups and generating evidence of what works to reduce inequalities. 50,51 The evidence produced by current research poorly represents those who are most disadvantaged. The SCHOPR principles call for co-produced, transdisciplinary research to create and deliver targeted national and local solutions to reduce inequalities. 33 More research is needed to develop and understand the implementation of evidence-based solutions drawing upon disciplines such as geography, anthropology, sociology, economics and history. Research capacity and skills must be embedded in the organisations which emerge from the latest restructure to help them become learning systems.

Redistributing resources and power to prevent illness and promote health
Inequalities are caused by the unequal distribution of social determinants of health, public and private investment, public sector workforce, services and power (the ability of one section of society to control another). 52 Without a fundamental change to how society can organise itself to address these, inequalities in health outcomes will persist. However, even within the way we organise ourselves currently and contrary to the sense that nothing can be done, there is evidence that the NHS can reduce inequalities. One example is an analysis of the increase of NHS resources to more deprived areas between 2001 and 2011, revealing a reduction in inequalities from causes amenable to healthcare. 53 This complements the principle of proportionate universalism, which states services should be accessible to all, but the intensity of the service should be proportionate to need with the most disadvantaged receiving more resources (Fig 3 ). 14 While existing national NHS allocation formulae are weighted for deprivation, evidence suggests they do not go far enough; and, in England, the weighting was reduced after the 2011 Act. 54
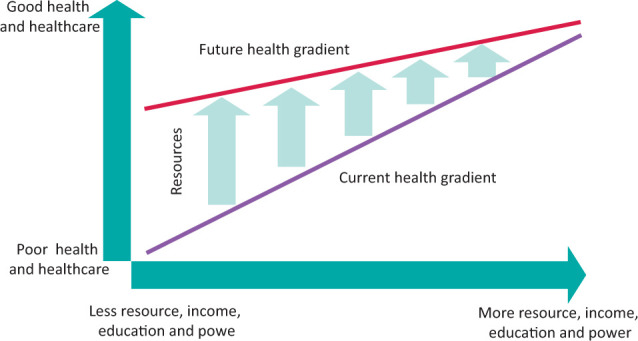
Distributing resources proportionate to need.
Beyond specific healthcare system evidence, there is also good evidence that cross government action can reduce inequalities. 22,23 Over the last couple of decades, there has been a natural experiment at a national scale. The UK government implemented a cross-government health inequalities programme and strategy from 2000 to 2010. Prior to the start of the programme, the difference in life expectancy between the most deprived areas and the rest of England was increasing by 0.57 months per year for males and 0.30 months per year for females. 22 The strategy reversed these trends with the gap in life expectancy reducing by 0.91 months per year for men and 0.50 months per year for women. Inequalities in the infant mortality rate (IMR) also decreased. 23 However, since the end of the strategy and the implementation of austerity, the inequality gap widened again by a similar amount as before and there is now evidence of increasing inequalities in IMR associated with rising rates of child poverty. 23 Key to the programme was a redistribution of funding, services and power to poorer areas, with regeneration initiatives, Sure Start centres to support early years childcare, increased NHS funding allocations, introduction of national minimum wage, more generous tax and benefit changes targeted at child poverty and targeted services in the most deprived local authorities. Unfortunately, detailed independent evaluation was not embedded or undertaken, and therefore the specific factors, either individually or collectively, which contributed to the observed narrowing inequalities gap remain unknown.
The importance of prevention and health promotion has been highlighted in several key documents. 24,34 The irony is that the under the Health and Social Care Act, public health was taken out of the NHS, but the current The NHS Long Term Plan prioritises prevention. Greater clarity is needed to ensure that the manner in which this emphasis is implemented does not unintentionally widen the gap. 55,56 For example, those with the resources and capabilities to benefit from an untargeted physical activity campaign have been and already are the more affluent groups with financial resources, health literacy and employment flexibility. This is also replicated within our research programmes and recruitment, which in many clinical research spheres do not represent diverse and disadvantaged communities. Policy makers should avoid the temptation to think that unhealthy lifestyles in people living in poorer areas arise because of a lack of knowledge or motivation and that the solution is information campaigns. 52,57 Decades of research reaching has demonstrated again and again that people, whether from poor or rich backgrounds, understand the determinants of health and have logical reasons for unhealthy choices. 57 For example, Graham found that pregnant women on low incomes still found money to buy cigarettes because smoking was the one opportunity in the day to do something for themselves in the context of very challenging life circumstances. 58 More recently, Thirlway found that smoking cessation was shaped by (lack of) social mobility. 59 To prevent illness and promote health we must break down the power hierarchies which suggest that one part of society knows what is best for another and get alongside people to understand why they act the way they do, treating them as experts in their lived experience, co-designing solutions as equal partners and advocating for the wider societal changes needed to address the social and economic context of inequality. 60
We all have an ethical and moral imperative to respond to the rapid proliferation of existing inequalities. Simultaneously, healthcare and public health organisations are being re-structured in England. We argue that the concept of health inequalities needs to be reframed to acknowledge the breadth of health and care inequalities with non-stigmatising language to ensure a systematic approach to the problem. A focus on building long-term equity-orientated organisational change in the NHS is urgently needed. At the core of any action should be the fundamental redistributions of resources, funding, workforce, services and power. If we do not act now in light of these stark inequalities, then when?
- 1. Public Health England . COVID-19: review of disparities in risks and outcomes. PHE, 2020. www.gov.uk/government/publications/covid-19-review-of-disparities-in-risks-and-outcomes [Accessed 09 June 2020]. [ Google Scholar ]
- 2. Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;74:964–8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Office for National Statistics . Deaths involving COVID-19 by local area and socioeconomic deprivation. ONS, 2020. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19bylocalareasanddeprivation/deathsoccurringbetween1marchand17april [Accessed 03 May 2020]. [ Google Scholar ]
- 4. APM Research Lab . The color of coronavirus: COVID-19 deaths race and ethnicity in the US. APM Research Lab, 2020. www.apmresearchlab.org/covid/deaths-by-race [Accessed Dec 29, 2020]. [ Google Scholar ]
- 5. Public Health England . Place-based approaches for reducing health inequalities: foreword and executive summary. PHE, 2019. www.gov.uk/government/publications/health-inequalities-place-based-approaches-to-reduce-inequalities/place-based-approaches-for-reducing-health-inequalities-foreword-and-executive-summary [Accessed 05 September 2019]. [ Google Scholar ]
- 6. World Health Organization . A framework for measuring health inequality. WHO, 1996. www.who.int/healthinfo/paper05.pdf [Accessed 29 December 2020]. [ Google Scholar ]
- 7. NHS Health Scotland . Health inequalities action framework. NHS, 2013. www.healthscotland.scot/media/1223/health-inequalities-action-framework_june13_english.pdf [Accessed 29 December 2020]. [ Google Scholar ]
- 8. Brooks D, Douglas M, Aggarwal N, et al. Developing a framework for integrating health equity into the learning health system. Learn Heal Syst 2017;1:e10029. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. NHS Confederation . Public reassurance needed over slow road to recovery for the NHS. NHS, 2020. www.nhsconfed.org/news/2020/06/road-to-recovery [Accessed 08 October 2020]. [ Google Scholar ]
- 10. Smith KE. Health inequalities in Scotland and England: the contrasting journeys of ideas from research into policy. Soc Sci Med 2007;64:1438–49. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Smith KE. The politics of ideas: The complex interplay of health inequalities research and policy. Sci Public Policy 2014;41:561–74. [ Google Scholar ]
- 12. Olivera J, Ford J, Sowden S, Bambra C. Conceptualisation of health inequalities by local health care systems: a document analysis. [Under peer review, 2021]. [ DOI ] [ PMC free article ] [ PubMed ]
- 13. Health and Social Care Act 2012. www.legislation.gov.uk/ukpga/2012/7/contents/enacted [Accessed 09 October 2019].
- 14. Marmot MG. Fair society, healthy lives: the Marmot review; strategic review of health inequalities in England post-2010. Marmot Review, 2010. [ Google Scholar ]
- 15. Acheson D. Independent inquiry into inequalities in health. Department of Health and Social Care, 1998. www.gov.uk/government/publications/independent-inquiry-into-inequalities-in-health-report [Accessed 29 December 2020]. [ Google Scholar ]
- 16. McIntosh Gray A. Inequalities in health. The black report: A summary and comment. Int J Heal Serv 1982;12:349–80. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Cookson R, Propper C, Asaria M, Raine R. Socio-Economic Inequalities in Health Care in England. Fisc Stud 2016;37:371–403. [ Google Scholar ]
- 18. Cheetham M, Moffatt S, Addison M, Wiseman A. Impact of Universal Credit in North East England: A qualitative study of claimants and support staff. BMJ Open 2019;9:29611. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Moffatt S, Lawson S, Patterson R, et al. A qualitative study of the impact of the UK ‘bedroom tax’. J Public Health (Oxf) 2016;38:197–205. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Lambert MF, Sowden S. Revisiting the risks associated with health and healthcare reform in England: Perspective of Faculty of Public Health members. J Public Health (Oxf) 2016;38:e438–45. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. NHS England . The NHS Long Term Plan. NHS, 2019. www.longtermplan.nhs.uk [Accessed 09 July 2019]. [ Google Scholar ]
- 22. Barr B, Higgerson J, Whitehead M. Investigating the impact of the English health inequalities strategy: Time trend analysis. BMJ 2017;358:j3310. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Robinson T, Brown H, Norman PD, et al. The impact of New Labour's English health inequalities strategy on geographical inequalities in infant mortality: A time-trend analysis. J Epidemiol Community Health 2019;73:564–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. NHS England . Second Phase of the NHS Response to COVID-19. NHS, 2020. www.gov.uk/government/publications/wuhan-novel-coronavirus [Accessed 03 May 2020]. [ Google Scholar ]
- 25. Brennan S. NHSE recommends law to abolish CCGs by 2022. HSJ; 2020. www.hsj.co.uk/commissioning/nhse-recommends-law-to-abolish-ccgs-by-2022/7029054.article [Accessed Nov 30, 2020]. [ Google Scholar ]
- 26. Alderwick H. NHS reorganisation after the pandemic. BMJ 2020;371:m4468. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Vize R. Controversial from creation to disbanding, via e-cigarettes and alcohol: an obituary of Public Health England. BMJ 2020;371:m4476. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Public Health England . Local action on health inequalities Understanding and reducing ethnic inequalities in health. PHE, 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/730917/local_action_on_health_inequalities.pdf [Accessed 10 September 2019]. [ Google Scholar ]
- 29. Public Health England, Institute of Health Equity . Promoting good quality jobs to reduce health inequalities. PHE, 2015. www.instituteofhealthequity.org/resources-reports/local-action-on-health-inequalities-promoting-good-quality-jobs-to-reduce-health-inequalities-/local-action-on-health-inequalities-promoting-good-quality-jobs-to-reduce-health-inequalities-full-report.pdf [ Google Scholar ]
- 30. Public Health England . Supporting the health system to reduce inequalities in screening PHE Screening inequalities strategy Public Health England leads the NHS Screening Programmes. PHE, 2018. https://phescreening.blog.gov.uk/wp-content/uploads/sites/152/2018/03/Supporting-the-health-system-to-reduce-inequalities-in-screening.pdf [Accessed 12 June 2019]. [ Google Scholar ]
- 31. Public Health England . Health Equity Assessment Tool [HEAT]. PHE, 2020. www.gov.uk/government/publications/health-equity-assessment-tool-heat [Accessed 10 November 2020]. [ Google Scholar ]
- 32. The Academy of Medical Sciences . Improving the health of the public by 2040. The Academy of Medical Sciences, 2016. [ Google Scholar ]
- 33. Strategic Coordination of the Health of the Public Research committee . Health of the public research principles and goals. SCHOPR, 2019. https://acmedsci.ac.uk/file-download/70826993 [Accessed 28 December 2020]. [ Google Scholar ]
- 34. The Academy of Medical Sciences . Future arrangements for prevention, health improvement and health protection. The Academy of Medical Sciences, 2020. https://acmedsci.ac.uk/file-download/90869115 [Accessed 29 December 2020]. [ Google Scholar ]
- 35. Royal College of Physicians . Inequalities in Health Alliance. RCP, 2020. www.rcplondon.ac.uk/projects/inequalities-health-alliance [Accessed 29 December 2020]. [ Google Scholar ]
- 36. Blackman T, Harrington B, Elliott E, et al. Framing health inequalities for local intervention: comparative case studies. Sociol Health Illn 2012;34:49–63. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Ford J. Director's appointment should be used to reframe the debate around health inequalities. HSJ; 2020. www.hsj.co.uk/leadership/directors-appointment-should-be-used-to-reframe-the-debate-around-health-inequalities/7028959.article [Accessed 29 December 2020]. [ Google Scholar ]
- 38. Green L. The concept of fatalism and New Labour's role in tackling inequalities. Br J Community Nurs 2001;6:106–11. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Schrecker T. Was Mackenbach right? Towards a practical political science of redistribution and health inequalities. Heal Place 2017;46:293–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Scott-Samuel A, Smith KE. Fantasy paradigms of health inequalities: Utopian thinking? Soc Theory Heal 2015;13:418–36. [ Google Scholar ]
- 41. Katz M. The Undeserving Poor: From the War on Poverty to the War on Welfare. New York: Pantheon, 1989. [ Google Scholar ]
- 42. Smith KE, Anderson R. Understanding lay perspectives on socioeconomic health inequalities in Britain: a meta-ethnography. Sociol Health Illn 2018;40:146–70. [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Parry J, Mathers J, Laburn-Peart C, Orford J, Dalton S. Improving health in deprived communities: What can residents teach us? Crit Public Health 2007;17:123–36. [ Google Scholar ]
- 44. Davidson R, Mitchell R, Hunt K. Location, location, location: The role of experience of disadvantage in lay perceptions of area inequalities in health. Heal Place 2008;14:167–81. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Mackenzie M, Collins C, Connolly J, Doyle M, McCartney G. Working-class discourses of politics, policy and health: ‘I don't smoke; I don't drink. The only thing wrong with me is my health’. Policy Polit 2017;45:231–49. [ Google Scholar ]
- 46. Bambra C, Norman P, Johnson NPAS. Visualising regional inequalities in the 1918 Spanish flu pandemic in England and Wales. Environ Plan A Econ Sp 2020. [ Google Scholar ]
- 47. Rich E, Miah A, Lewis S. Is digital health care more equitable? The framing of health inequalities within England's digital health policy 2010–2017. Sociol Health Illn 2019;41:31–49. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Sowden SL, Raine R. Running along parallel lines: How political reality impedes the evaluation of public health interventions. A case study of exercise referral schemes in England. J Epidemiol Community Health 2008;62:835–41. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Sadare O, Williams M, Simon L. Implementation of the Health Equity Impact Assessment [HEIA] tool in a local public health setting: challenges, facilitators, and impacts. Can J Public Heal 2020;111:212–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Cookson R, Griffin S, Norheim O, Culyer A. Distributional cost-effectiveness analysis. Oxford University Press, 2020. [ Google Scholar ]
- 51. Pons-Vigués M, Diez È, Morrison J, et al. Social and health policies or interventions to tackle health inequalities in European cities: A scoping review. BMC Public Health 2014;14:198. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 52. McCartney G, Collins C, Mackenzie M. What [or who] causes health inequalities: Theories, evidence and implications? Health Policy 2013;113:221–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Barr B, Bambra C, Whitehead M, Duncan WH. The impact of NHS resource allocation policy on health inequalities in England 2001-11: Longitudinal ecological study. BMJ 2014;348:g3231. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 54. Levene LS, Baker R, Bankart J, Walker N, Wilson A. Socioeconomic deprivation scores as predictors of variations in NHS practice payments: A longitudinal study of English general practices 2013-2017. Br J Gen Pract 2019;69:E546–54. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 55. Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. JECH 2013;67:190–3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations? In: Babones S. (ed). Social inequality and public health. Policy Press, 2009:64–81. [ Google Scholar ]
- 57. Kelly MP, Barker M. Why is changing health-related behaviour so difficult? Public Health 2016;136:109–16. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. Graham H. Women, Smoking and Disadvantage. In: Slama K. (ed). Tobacco and health. Springer, 1995:695–7. [ Google Scholar ]
- 59. Thirlway F. Explaining the social gradient in smoking and cessation: the peril and promise of social mobility. Sociol Health Illn 2020;42:565–78. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 60. Cheetham M, Gorman S, Gibson E, Wiseman A. It's not about telling people to eat better, stop smoking or get on the treadmill. In: Newbury-Birch D, Allan K. Co-creating and co-producing research evidence. Routledge, 2019:66–77. [ Google Scholar ]
- View on publisher site
- PDF (157.0 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Systematic review of the effectiveness of the health inequalities strategy in England between 1999 and 2010
Ian holdroyd, alice vodden, akash srinivasan, clare bambra, john alexander ford.
- Author information
- Article notes
- Copyright and License information
Correspondence to Dr John Alexander Ford; [email protected]
Corresponding author.
Series information
Original research
Received 2022 Mar 22; Accepted 2022 Aug 12; Collection date 2022.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
The purpose of this systematic review is to explore the effectiveness of the National Health Inequality Strategy, which was conducted in England between 1999 and 2010.
Three databases (Ovid Medline, Embase and PsycINFO) and grey literature were searched for articles published that reported on changes in inequalities in health outcomes in England over the implementation period. Articles published between January 1999 and November 2021 were included. Title and abstracts were screened according to an eligibility criteria. Data were extracted from eligible studies, and risk of bias was assessed using the Risk of Bias in Non-randomized Studies of Interventions tool.
The search strategy identified 10 311 unique studies, which were screened. 42 were reviewed in full text and 11 were included in the final review. Six studies contained data on inequalities of life expectancy or mortality, four on disease-specific mortality, three on infant mortality and three on morbidities. Early government reports suggested that inequalities in life expectancy and infant mortality had increased. However, later publications using more accurate data and more appropriate measures found that absolute and relative inequalities had decreased throughout the strategy period for both measures. Three of four studies found a narrowing of inequalities in all-cause mortality. Absolute inequalities in mortality due to cancer and cardiovascular disease decreased, but relative inequalities increased. There was a lack of change, or widening of inequalities in mental health, self-reported health, health-related quality of life and long-term conditions.
Conclusions
With respect to its aims, the strategy was broadly successful. Policymakers should take courage that progress on health inequalities is achievable with long-term, multiagency, cross-government action.
Trial registration number
This study was registered in PROSPERO (CRD42021285770).
Keywords: public health, health policy, quality in health care
Strengths and limitations of this study.
This is the first study to synthesise all published studies and grey literature on the health inequalities strategy conducted in England from 1999 to 2010.
This study used a broad search strategy of peer-reviewed and grey literature.
The retrospective nature of studies and lack of counterfactual means that causal claims as to the effect of the strategy cannot easily be made. This resulted in an increased risk of bias of studies.
Introduction
The pandemic has exacerbated societal health inequalities, with higher numbers of COVID-19 related cases and deaths in areas of higher socioeconomic disadvantage and among minority ethnic groups. 1 2 In England, the COVID-19 mortality rate for those under 65 was 3.7× greater in the most deprived 10% of local areas compared with the least deprived. Age-standardised COVID-19 mortality rates were more than twice as high in the most deprived 10% of areas compared with the least. 2
Knowledge of the existence of health inequalities is not new. The first major UK publication describing health inequalities was the Black report in 1980, although health inequalities had been described and debated in the academic literature for decades before that. It was not until 1997, with a newly elected government, that health inequalities became a policy priority. The government commissioned a health inequalities review, subsequently published in 1998 as the Acheson report, and committed itself to implement the evidence-based policy recommendations. 3 Subsequently, a wide-ranging national health inequalities strategy was implemented, with various strategies and aims updated over time. This was the first and most extensive international attempt to address health inequalities through a widespread programme of cross-government action.
Two national documents set out the health inequalities strategy. First, ‘Reducing health inequalities: an action report’ was published in 1999 in response to the Acheson report. It described a wide variety of policies designed to reduce health inequalities: both more ‘downstream’ initiatives, such as increased National Health Service (NHS) funding or the establishment of a National Institute for Clinical Excellence, and more ‘upstream’ policies, such as a national minimum wage, the new deal for employment and increased funding for schools, housing and transport. 4 Second, ‘Tackling health inequalities: a Program for Action’ was published in 2003. 5 It set out 82 cross-departmental commitments, along with 12 headline indicators of the key areas to be monitored. Again, these commitments included a range of ‘upstream’ and ‘downstream’ policies. Other studies have previously summarised the strategy. 6–8 The strategy involved a wide range of policy actions across different sectors. These included large increases in levels of public spending on a range of social programmes (such as the introduction of the Child Tax Credit; SureStart Children’s Centres), the introduction of the national minimum wage, area-based interventions such as the Health Action Zones and Neighbourhood Renewal funds and a substantial increase in expenditure on the NHS. The latter was targeted at more deprived neighbourhoods when, after 2001, a ‘health inequalities weighting’ was added to the way in which NHS funds were geographically distributed, so that areas of higher deprivation received more funds per head to reflect higher health need. 9
The programme for action included two national targets: (1) by 2010, to reduce by at least 10% the gap in infant mortality between routine and manual groups and the population as a whole and (2) by 2010, to reduce by at least 10% the gap between the fifth of areas with the lowest life expectancy at birth and the population as a whole. The ‘areas with the lowest life expectancy at birth and the population as a whole’ were defined by later documents as the ‘Spearhead areas’. 10–12 These 70 local authority areas were identified as being the worst performing local authorities associated with three or more of: male and female life expectancy at birth, cancer and cardiovascular disease mortality rates for the under 75s and Index of Multiple Deprivation (IMD) 2004 scores. These targets were based on relative, rather than absolute, inequalities. 12 13 This is important as debate exists as to which of these is the most appropriate measure of inequality. 3 14 15 Absolute inequalities measure the numerical gap between groups, while relative inequalities measure the percentage difference between groups.
One major criticism of health inequalities research and policy is that there has been too much effort put into describing the problem, rather than finding solutions. The National Health Inequalities Strategy in England 1999–2010 provides a key international example of the latter. It is a high-profile international case study of long term multifaceted government action. Discussions to date of the effects of the strategy have been polarised, with some prominent commentators arguing that it failed, 8 while others have asserted that it was effective. 16 17 This is partly because early evaluations of this health inequalities strategy suggested that it had failed to reach its targets and that inequalities may have increased during this period. 8 10 16 18 However, subsequent research found that this period was associated with a reduction in health inequalities. 6 9 19–21 As governments around the world consider how to respond to inequalities compounded by the pandemic, here we present a systematic review of the studies assessing the effectiveness of this health inequalities strategy.
This systematic review was conducted in accordance with established methodology 22 and reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. 23 This systematic review was registered with PROSPERO (CRD42021285770).
Search strategy and selection criteria
Three electronic databases (Ovid Medline, Ovid Embase and Ebsco PsycINFO) were systematically searched from January 1999 to November 2021. The search terms were based in part on previous literature, which identified key search terms to identify studies investigating inequality and inequity 24 and the UK. 25 Online supplemental table 1 presents the search terms. After removing duplicate records, abstracts and titles were screened according to the eligibility criteria by two researchers (IH and AS) using the software Rayyan by December 2021. Discrepancies were resolved by a third researcher (JAF). Each researcher cross screened 20% of the abstracts and titles of the other to ensure accuracy. Three conflicts arose, which were resolved after discussion. A detailed grey literature search of the UK Government Web Archives, specific websites (such as the King’s Fund) and a broad search using an internet search engine (Google) was used. Relevant citations of included studies were also screened.
bmjopen-2022-063137supp001.pdf (144.9KB, pdf)
Inclusion criteria were:
Studies assessing the impact of the health inequalities strategy in England between 1999 and 2010 on inequality in health outcomes in England.
Any form of quantitative study.
Studies reporting primary research.
Studies in any language.
Exclusion criteria were:
Studies whose methodology make it impossible to draw conclusions about the impact of the strategy.
Studies that reported non-health inequalities.
Earlier editions of included reports.
The full text of all articles screened as meeting the eligibility criteria or possibly meeting the criteria were reviewed. The following information was independently extracted from each study by two authors (IH and AV): first author, year of publication, aim, design, data sources, time period of analysis, population, health inequalities measured, main findings and risk of bias. The main outcomes of interest were absolute or relative changes in socioeconomic inequalities in life expectancy and infant mortality in the population of England between 1999 and 2010 to reflect the aims of the strategy. All results compatible with each outcome domain were sought from each study. Secondary outcomes included changes to socioeconomic inequalities in mortality, comorbidities or self-reported health.
Quality assessment
Risk of bias was assessed at a study level using the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool, which assesses the risk of bias across seven domains. One author (IH) undertook the risk of bias assessment, and this was double checked by a second author (AS or AV) with disagreements resolved by a third (JAF).
Patient and public involvement
Patients were not involved in the design or execution of this study. Nor were members of the public.
Due to the small number of studies with a large amount of data heterogeneity, it was deemed inappropriate to perform a meta-analysis. Instead, studies were synthesised narratively.
After removal of duplicates, the search identified 10 311 unique records. Forty-two were reviewed in full text, and 11 were included in the final review. A flow diagram of the screening and selection process can be found in figure 1 . Six studies contained data on inequalities of life expectancy or mortality, 6 7 9 10 12 19 three on disease-specific mortality, 10 12 26 three on infant mortality 10 13 21 and three on morbidities. 7 20 27 Six studies investigated geographical health inequalities, four investigated health inequalities at an individual level and one had statistics from both measures. Measures of socioeconomic status included income, living in a spearhead area, deprivation, occupation, social class and education. Data were collected between 1983 and 2017 ( table 1 ). Results from these papers are summarised in table 2 . Table 3 shows the risk of bias of each study across seven domains.
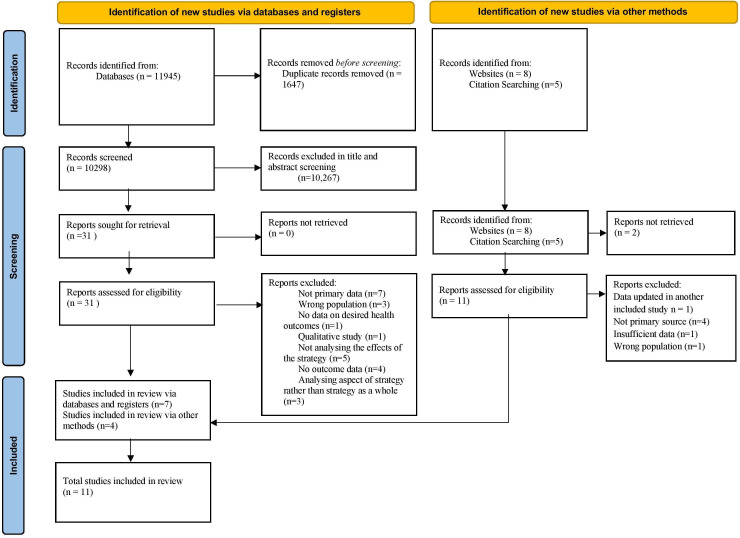
Study selection process.
Study characteristics
ONS, Office for National Statistics.
Study findings
Risk of bias – ROBINS-I tool
NI, No Information; ROBINS-I, Risk of Bias in Non-randomized Studies of Interventions.
Life expectancy, all-cause mortality and disease-specific mortality
Six studies reported data on life expectancy or mortality. Two earlier studies reported a widening of inequalities in life expectancy with one showing narrowing of mortality inequalities. The four more recent studies showed a narrowing of inequalities.
Two early government reports showed widening of life expectancy inequalities and mixed results for mortality inequalities. ‘Tackling Health Inequalities: 2007 Status Report on the Programme for Action’ used Office for National Statistics (ONS) data based on life estimates made using the 2006 census. It compared life expectancy in spearhead areas and the rest of the country. While life expectancy had increased for both spearhead and non-spearhead areas, absolute and relative inequalities between them had increased between 1995–1997 and 2004–2006. 10 The second reported ONS data up to and including 2010. 12 Compared with the 1995–1997 baseline, the absolute and relative gap in life expectancy between spearhead areas and England as a whole increased by 2008–2010.
Four later published studies found that inequalities had narrowed. The first study by Barr and colleagues 9 compared individuals living in the fifth most deprived areas to those living in the fifth least deprived areas. The authors found that inequalities of healthcare amenable mortality, defined as mortality from causes that would be prevented provided appropriate access to high-quality healthcare, narrowed between 2001 and 2011. Absolute inequalities for men and women fell with 85% of the change explained by redistributive resource allocation changes between areas. The relative gap narrowed for males and females. However, the authors found that absolute or relative inequalities of mortality not amenable to healthcare failed to change noticeably between 2001 and 2011. 9
The second study by Barr and colleagues 6 investigated geographical inequalities between 1983 and 2015 using ONS data based on the 2011 census, rather than 2006, which informed earlier government publications. They analysed trends in the absolute difference of life expectancy and mortality in the 20% most deprived local authorities compared with the rest of England. Supplementary analysis compared life expectancy in spearhead and non-spearhead areas. The authors identified breakpoints to account for the lag between implementation and outcomes. Both socioeconomic inequalities and inequalities between spearhead and non-spearhead areas in life expectancy for men and women statistically significantly increased year-on-year before the strategy and decreased during the time of the strategy, with no evidence that this decrease continued after the strategy. Relative socioeconomic inequalities in mortality fell year-on-year throughout the strategy for both men and women and increased before and after the strategy for men. Further analysis showed that the gap in life expectancy between spearhead areas and the rest of the country did not decrease until after 2005. Relative socioeconomic inequalities in life expectancy widened before and after the strategy period and narrowed during it. The authors found that using population estimates using the 2006 census caused an artificial increase in life expectancy inequalities compared with 2011 estimates.
Hu and colleagues 7 compared data from the health survey for England to similar surveys done in other European countries. They investigated trends in inequalities of all-cause mortality between those with high (tertiary) education and the rest of the country. The gap narrowed more significantly in 2000–2010 compared with 1990–2000 in England.
While aforementioned studies, analysing differences between the most and least deprived areas, are important concerning the strategies aims, they fail to describe the change in the social gradient across the whole of the population. Buck and Maguire 19 examined the relationship between area-based income deprivation and life expectancy, comparing data from 1999 to 2003 to 2006–2010. The authors found improved life expectancy for all levels of deprivation but a greater improvement in more deprived areas. It was noted that both unemployment and older people’s deprivation played a particularly important role in determining differences in life expectancy between areas.
Three studies reported changes in inequalities in disease-specific mortality. Two government documents examined inequalities in mortality due to cancer between spearhead areas and England as a whole from 1995 to 1997 to 2006–2008 and 2008–2010 using ONS data. By 2006–2008, absolute inequalities fell, without a change in relative inequalities. 10 By 2010, the absolute gap had fallen further, with an increase in the relative gap. 12 Absolute inequalities in mortality due to circulatory disease decreased by 2006–2008, but relative inequalities widened. By 2008–2010, there was a further decrease in absolute but an increase in relative inequalities. Exarchakou and colleagues 26 reported inequalities of 1-year survival rate following a diagnosis of one of the 24 most common cancers between 1996 and 2013. They investigated the absolute difference between individuals living in the fifth most and fifth least deprived areas. The gap narrowed in only 6 of 20 cancers in men and 2 of 21 cancers in women and widened for three cancers (two in women and one in men). One final study examined inequalities in road accident causality in the fifth most deprived local authority districts areas compared with England as a whole. 10 The absolute gap decreased between 1998 and 2006.
Infant mortality
Three studies reported changes in the infant mortality rate. Initial reporting using ONS data from 2004 to 2006 found that inequalities had widened between routine plus manual groups and the population as a whole compared with the 1997–1999 baseline. 10 A later report found that by 2008–2010, inequalities had narrowed compared with the baseline. 13 Robinson and colleagues 21 calculated the infant mortality rate in 323 lower tier local authorities between 1983 and 2017 to investigate changes in inequalities between the 20% most deprived areas and the rest of the country. Absolute inequality increased year on year before the strategy and decreased during it. A non-significant increase was seen after the strategy ended. Relative inequalities marginally decreased during the time of the strategy, in contrast to an increase that was seen before and after the strategy period.
Morbidities
Three studies reported on morbidities using Health Survey of England data. Specifically, these studies investigated self-assessed health, health-related quality of life, mental health and long-term health. The Health Survey of England contains data collected from a nationally representative sample of those residing at private residential addresses and has been carried out since 1991. 28 Around 8000 adults and 2000 children take part in the survey each year.
Mixed results were found concerning self-reported health. Between 1996 and 2009, the probability of reporting bad or very bad health remained relatively constant for those in the highest social class but increased for those in lower social classes. 27 When comparing those with high and low education, there was no significant difference in inequality trends between 2000 and 2010 compared with 1990–2000. Additionally, there was no significant difference in the change of these trends between these periods compared with three European countries. 7 Costa Font and colleagues 20 measured inequalities in self-reported health using concentration indices, whereby a high result indicates more inequality. Equalised household income was used to measure inequality across the whole population. In contrast to the two aforementioned studies, they reported a fall in the concentration index between 1997 and 2007, indicating a reduction in inequality.
Health-related quality of life did not change between social classes from 1996 to 2008. 27 When assessed by a concentration index comparing different household incomes, inequalities of long-term health problems increased between 1997 and 2007. 20 There was no significant change in the trend of inequalities of long-term health problems by education in 2000–2010 compared with 1990–2000. Nor was there a significant difference in the change in trend in England compared with three European countries. 7 While mental health improved in all social classes between 1997 and 2009, it did so more for individuals in higher social classes. 27
Principle findings
There is evidence that the strategy met the infant mortality target, while the life expectancy target was reached for men but not women. Absolute health inequalities in life expectancy, mortality, infant mortality and multiple major causes of death reduced. Less evidence is available concerning relative inequalities. More recent data suggest that relative socioeconomic inequalities in life expectancy and infant mortality narrowed. Relative inequalities of mortality narrowed between the fifth most deprived areas and the country as a whole, but not between the fifth most and fifth least deprived areas. The only data available on disease-specific conditions suggest an increase in relative inequalities. This may be due to a lack of newly published studies, using more recent census data and sampling from the later years of the strategy being available as it is for life expectancy and infant mortality. The difference may also be due to the statistical relationship whereby relative inequalities may increase as a result of a fall in absolute inequalities. 29 30 There was a lack of change or worsening of change for inequalities in mental health, health-related quality of life and long-term conditions. This lack of change or increased inequality for self-reported health measures may be due to multiple reasons. As all studies used the same survey, with data collected shortly after the 2008 financial crash, perceptions of economic security may have altered results. It may be that self-reported measures are more resilient to change. Alternatively, small changes in categorically assessed self-assessed measures may be less easily observed compared with life expectancy and infant mortality that are continuous measures. Health inequalities were found to have narrowed more consistently when measured between geographical areas rather than between individuals. This may be due to longer follow-up periods in many of the studies that were measured at a geographical level, extending beyond the immediate aftermath of the banking crises. Alternatively, it could have been caused by the redistributive resource allocation changes that occurred between areas. 9
Strengths and limitations
This is the first study to collate and synthesise all evidence of the first international attempt at a cross-government strategy to address health inequalities. We used an extensive search strategy with robust screening, data extraction and quality assessment processes. We included peer-reviewed articles and grey literature, including documents published at the time and identified through the UK government archives.
The main limitation is that the studies included are retrospective using either time-trend or before and after methods. All of the studies have a high risk of bias due to deviations from intended interventions. This was predominantly because of the lack of a robust counterfactual that makes it difficult to unpick the impact of the strategy against the impact of other factors, such as broad economic growth before the financial crash in 2008. These limitations are common to any attempt to assess the impact of national policy; however, considering the breadth and ambition of the strategy it is disappointing that more comprehensive evaluations or data are not available. The strategy’s wide-ranging nature does however allow many of these factors to be considered a part of it rather than as a confounding factor. For example, the large decrease in poverty rates, especially in children 31 and pensioners, 32 may both have contributed. Additionally, not every abstract was double screened. However, 40% of abstracts were cross checked to ensure consistency, and only three discrepancies arose, none of which were included in the review.
The included articles use different measures that make direct comparisons impossible, for example, comparing the most deprived areas to either the least deprived areas or the rest of the population and using individual-level measures of socio-economic status (eg, occupation) or area-based measures (eg, IMD). Morbidity data are based on self-reported measures within a nationally representative survey, rather than chronic disease registers.
As indicated by guidance, absolute and relative inequalities were included. 14 33 This aligns with existing guidance and debate both from those who argue that absolute inequalities are the more important measure for policymakers 3 and others who support the idea that relative inequalities are also of significant importance. 34
What this research means
A lack of progress on health inequalities, despite policy priority, can lead to a sense of fatalism and powerlessness to effect change. These findings are therefore important because they show that with sustained cross-government action, progress on health inequalities is possible. It is particularly encouraging that improvements were made in both of the areas that the strategy predominantly set out to improve: inequalities in life expectancy and infant mortality.
These results are even more encouraging when considering that they came from a strategy that was far from perfect. Critics have noted various points about the strategy, for example, that it was insufficiently based on reliable evidence, 8 18 35 36 flawed in delivery, 8 16 18 insufficiently focused on the wider determinants of health 16 34 37 and that efforts may not have been large enough. 8 34 38
Earlier findings consistently showed no improvement in life expectancy inequalities, yet later results were more positive. This may be due to a lag period between the implementation of the strategy of interventions and changes in health outcomes. Certain initiatives would take considerably longer to impact inequalities in life expectancy, such as reducing childhood poverty, compared with more downstream factors, such as blood pressure control. Alternatively, it may be due to more accurate and up-to-date data, such as the 2011 census. Importantly, this shows that sufficient time is needed between implementation and measuring outcomes.
Implications for policy and research
Governments around the world are taking steps to address health inequalities, particularly in light of the growing evidence of an unequal pandemic. 39 For example, the UK government has committed to a programme of ‘levelling up’ regional inequalities and setting out new legislation to address health inequalities. This review suggests that it is possible to reduce health inequalities through long-term cross-government action, which was wide reaching both in terms of government departments and across the life course. Most encouragingly with respect to current government aims, geographical health inequalities especially narrowed. The strategy was supported by significant increases in both funding and reform of public services, of which only one has continued. Since the end of the strategy period, public services internationally, but particularly in the UK, have experienced reduced funding as a result of austerity policies from 2010 onwards. In the UK, this has particularly impacted on local authorities, social security, children’s services and, until the pandemic, to the NHS. Indeed, there is evidence that from 2010 onwards (and before the unequal impact of the pandemic) the improvements in health inequalities under the English strategy have reversed with, for example, increasing inequalities in infant mortality rates 40 and falling life expectancy in the most deprived areas. 41 Considerable investments in these services would be necessary to recreate a proactive attempt to tackle the social determinants of health inequalities.
The strategy used relative measures of inequality. Absolute measures are easier to change, making them appealing to policymakers as progress can be more easily proven. The goals were based on long-term changes in life expectancy and infant mortality rather than shorter term changes in measures such as blood pressure and heart rate. These were appropriate for the strategy given the wide-ranging, cross-departmental approach that aimed to target determinants of ill health. The fact that long-term, ambitious health inequalities targets require a cross-departmental approach can be of benefit to policy makers. They can provide rationale and strengthen the argument for a wide range of potentially transformative policies that may otherwise fail to be enacted due to a lack of political support. Goals were based on changes between the most and least deprived areas, rather than changes in the societal gradient in health. This again would be an easier target for policymakers to achieve. The government’s current targets, through the ‘levelling up’ programme are less ambitious than the strategy’s. 42 Only an absolute narrowing in life expectancy and well-being is aimed for, rather than the 10% change targeted by the strategy. Additionally, the absolute gap in life expectancy by area is measured between the top and bottom 10% rather than 20%.
Arguably more policy priority should have been given to reducing the gap in morbidities as the data fail to show a convincing narrowing of inequalities of self-reported health, mental health, health-related quality of life and long-term conditions.
More research is needed to unpick the active ingredients and exact initiatives that were most effective during the strategy. This should start with a more detailed understanding of which diseases drove the reduction in life expectancy and a broader understanding of how the wider determinants of health such as housing, income and education may have impacted changes in infant mortality, mortality and life expectancy.
In summary, this review found some evidence that the 1999–2010 cross-government health inequalities strategy led to a reduction in the absolute inequalities in life expectancy, mortality, infant mortality and major causes of death. While the impact on relative inequalities is less clear, there seemed to be a narrowing of relative inequalities in at least life expectancy and infant mortality. The national targets relating to life expectancy were met for men, but not women, and were achieved for infant mortality. Policymakers should take courage that progress on health inequalities is achievable with long-term, multiagency, cross-government action. These findings are especially pertinent at present times whereby many governments are aiming to use postpandemic recovery as an opportunity to build back better.
Supplementary Material
Twitter: @ilk21
Contributors: JAF conceptualised the study. JAF and IH drafted the protocol, and IK and AV provided comments. IK developed the searches with the support of IH and JAF. IH and AS screened the titles and abstract and were supported by JAF. IH and JF screened the full text articles. IH, AS and AV extracted and checked the extraction. IH wrote the first draft of the manuscript. JAF, IK, CB, AS and AV redrafted. All authors approved the final version. JAF is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study.
Ethics statements
Patient consent for publication.
Not applicable.
- 1. Bambra C, Riordan R, Ford J, et al. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;74:jech-2020-214401. 10.1136/jech-2020-214401 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Suleman M, Sonthalia S, Webb C. Unequal pandemic, fairer recovery: the COVID-19 impact inquiry report. The Health Foundation 2021. [ Google Scholar ]
- 3. Department of Health . Independent inquiry into inequalities in health (the Acheson report) 1998.
- 4. Department of Health . Reducing health inequalities: an action report 1999.
- 5. Department of Health . Tackling health inequalities: a program for action 2003.
- 6. Barr B, Higgerson J, Whitehead M. Investigating the impact of the English health inequalities strategy: time trend analysis. BMJ 2017;358:j3310. 10.1136/bmj.j3310 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Hu Y, van Lenthe FJ, Judge K, et al. Did the English strategy reduce inequalities in health? A difference-in-difference analysis comparing England with three other European countries. BMC Public Health 2016;16:865. 10.1186/s12889-016-3505-z [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Mackenbach JP. Has the English strategy to reduce health inequalities failed? Soc Sci Med 2010;71:1249–53. 10.1016/j.socscimed.2010.07.014 [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Barr B, Bambra C, Whitehead M. The impact of NHS resource allocation policy on health inequalities in England 2001-11: longitudinal ecological study. BMJ 2014;348:g3231. 10.1136/bmj.g3231 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Department of Health . Tackling health inequalities: 2007 status report of the program for action 2007.
- 11. Department of Health . Tackling health inequalities: 10 years on 2009.
- 12. Department of Health . Mortality monitoring Bulletin. Life expectancy, all-age-all-cause mortality, and mortality from selected causes, overall and inequalities. Update to include data for 2010 2011.
- 13. Department of Health . Mortality monitoring Bulletin (infant mortality inequalities): update to include data for 2010 2011.
- 14. King NB, Harper S, Young ME. Use of relative and absolute effect measures in reporting health inequalities: structured review. BMJ 2012;345:e5774. 10.1136/bmj.e5774 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Low A, Low A. Importance of relative measures in policy on health inequalities. BMJ 2006;332:967–9. 10.1136/bmj.332.7547.967 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Department of Health . Fair society, healthy lives (the Marmot review) 2010. [ DOI ] [ PubMed ]
- 17. Marmot M. Health equity in England: the Marmot review 10 years on. BMJ 2020;368:m693. 10.1136/bmj.m693 [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Mackenbach JP. Can we reduce health inequalities? An analysis of the English strategy (1997-2010). J Epidemiol Community Health 2011;65:568–75. 10.1136/jech.2010.128280 [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Buck D, Maguire D. Inequalities in life expectancy: changes over time and implications for policy 2015;76. [ Google Scholar ]
- 20. Costa Font J, Hernández-Quevedo C, McGuire A. Persistence despite action? Measuring the patterns of health inequality in England (1997-2007). Health Policy 2011;103:149–59. 10.1016/j.healthpol.2011.07.002 [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Robinson T, Brown H, Norman PD, et al. The impact of new labour's English health inequalities strategy on geographical inequalities in infant mortality: a time-trend analysis. J Epidemiol Community Health 2019;73:564–8. 10.1136/jech-2018-211679 [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Higgins J, Thomas J, Chandler J. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane 2021. [ Google Scholar ]
- 23. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Prady SL, Uphoff EP, Power M, et al. Development and validation of a search filter to identify equity-focused studies: reducing the number needed to screen. BMC Med Res Methodol 2018;18:106. 10.1186/s12874-018-0567-x [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Ayiku L, Levay P, Hudson T, et al. The medline UK filter: development and validation of a geographic search filter to retrieve research about the UK from OVID medline. Health Info Libr J 2017;34:200–16. 10.1111/hir.12187 [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Exarchakou A, Rachet B, Belot A, et al. Impact of national cancer policies on cancer survival trends and socioeconomic inequalities in England, 1996-2013: population based study. BMJ 2018;360:k764. 10.1136/bmj.k764 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Maheswaran H, Kupek E, Petrou S. Self-reported health and socio-economic inequalities in England, 1996-2009: repeated national cross-sectional study. Soc Sci Med 2015;136-137:135–46. 10.1016/j.socscimed.2015.05.026 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Mindell J, Biddulph JP, Hirani V, et al. Cohort profile: the health survey for England. Int J Epidemiol 2012;41:1585–93. 10.1093/ije/dyr199 [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Harper S, King NB, Meersman SC, et al. Implicit value judgments in the measurement of health inequalities. Milbank Q 2010;88:4–29. 10.1111/j.1468-0009.2010.00587.x [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Scanlan JP. Guest editorial. Chance 2006;19:47–51. 10.1080/09332480.2006.10722787 [ DOI ] [ Google Scholar ]
- 31. Department for Work and Pensions Department for Education . Child poverty in the UK: the report on the 2010 target 2012.
- 32. Office for National Statistics . Chapter 13: inequalities and poverty in retirement. In: Pension trends: compendium, 2014. [ Google Scholar ]
- 33. Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med 1997;44:757–71. 10.1016/S0277-9536(96)00073-1 [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Law C, Parkin C, Lewis H. Policies to tackle inequalities in child health: why haven't they worked (better)? Arch Dis Child 2012;97:301–3. 10.1136/archdischild-2011-300827 [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Bambra C, Smith KE, Garthwaite K, et al. A labour of Sisyphus? Public policy and health inequalities research from the Black and Acheson Reports to the Marmot Review. J Epidemiol Community Health 2011;65:399–406. 10.1136/jech.2010.111195 [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Macintyre S, Chalmers I, Horton R, et al. Using evidence to inform health policy: case study. BMJ 2001;322:222–5. 10.1136/bmj.322.7280.222 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Hunter DJ, Popay J, Tannahill C, et al. Getting to grips with health inequalities at last? BMJ 2010;340:c684. 10.1136/bmj.c684 [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Bambra C. Health divides: where you live can kill you 2016:192–7.
- 39. Bambra C, Lynch J, Smith KE. The unequal pandemic: COVID-19 and health inequalities. Policy Press, 2021. [ Google Scholar ]
- 40. Taylor-Robinson D, Lai ETC, Wickham S, et al. Assessing the impact of rising child poverty on the unprecedented rise in infant mortality in England, 2000-2017: time trend analysis. BMJ Open 2019;9:e029424. 10.1136/bmjopen-2019-029424 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Raleigh VS, Goldblatt P. Life expectancy in England: what’s going on? BMJ 2019. [ Google Scholar ]
- 42. HM Government . Levelling up the United Kingdom: missions and metrics technical Annex 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data availability statement.
- View on publisher site
- PDF (1.7 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
- Collections Home
- About Collections
- Browse Collections
- Calls for Papers
Health Inequities and Disparities Research
PLOS ONE is proud to publish the Health Inequities and Disparities Collection. Launched in September 2019, this Call for Papers welcomed articles on all relevant disciplines in the field of public health tackling health inequities and disparities. The resulting collection, in the words of one of our Guest Editors, Professor Diana Burgess, "features cutting-edge papers that tackle health inequities and disparities by researchers from a variety of disciplinary perspectives. The collection is truly international in scope and addresses a broad range of health inequities, rooted in historic and contemporary laws, policies, and practices, which disadvantage certain groups. These papers include health equities due to race/ethnicity, socio-economic status, sexual or gender minority identification, immigrant status (including undocumented immigrants), incarceration, socio-economic status, and country of residence. This thought-provoking collection is an important contribution to the field of health inequities and disparities and will expand our understanding of how we define and study these topics."
Image Credit: Tama66
- Guest Editors
- PLOS ONE Collection
- Image credit PLOS ONE Clare Bambra Clare Bambra August 10, 2020 Guest Editor, PLOS ONE
- Image credit PLOS ONE Hans Bosma Hans Bosma August 10, 2020 Guest Editor, PLOS ONE
- Image credit PLOS ONE Diana Burgess Diana Burgess August 10, 2020 Guest Editor, PLOS ONE
- Image credit PLOS ONE Jennie Popay Jennie Popay August 10, 2020 Guest Editor, PLOS ONE
- Image credit PLOS ONE Joseph Telfair Joseph Telfair August 10, 2020 Guest Editor, PLOS ONE
- Image credit PLOS ONE Barbara Turner Barbara Turner August 10, 2020 Guest Editor, PLOS ONE
- Image credit Hamilton Viana Viana PLOS ONE Racial/ethnic inequities in the associations of allostatic load with all-cause and cardiovascular-specific mortality risk in U.S. adults February 13, 2020 Luisa N. Borrell, Elena Rodríguez-Álvarez, Florence J. Dallo
- Image credit Rinck Content Studio PLOS ONE Associations between interrelated dimensions of socio-economic status, higher risk drinking and mental health in South East London: A cross-sectional study February 14, 2020 Sadie Boniface, Dan Lewer, Stephani L. Hatch, Laura Goodwin
- Image credit Mahdiar Mahmoodi PLOS ONE Relationship of sociodemographic and lifestyle factors and diet habits with metabolic syndrome (MetS) among three ethnic groups of the Malaysian population March 19, 2020 Saleem Perwaiz Iqbal, Amutha Ramadas, Quek Kia Fatt, Ho Loon Shin, Wong Yin Onn, Khalid Abdul Kadir
- Image credit Joy Real PLOS ONE Changing relative and absolute socioeconomic health inequalities in Ontario, Canada: A population-based cohort study of adult premature mortality, 1992 to 2017 April 2, 2020 Emmalin Buajitti, John Frank, Tristan Watson, Kathy Kornas, Laura C. Rosella
- Image credit Kevin McCutcheon PLOS ONE Inequalities in education and national income are associated with poorer diet: Pooled analysis of individual participant data across 12 European countries May 7, 2020 H. L. Rippin, J. Hutchinson, D. C. Greenwood, J. Jewell, J. J. Breda, A. Martin, D. M. Rippin, K. Schindler, P. Rust, S. Fagt, J. Matthiessen, E. Nurk, K. Nelis, M. Kukk, H. Tapanainen, L. Valsta, T. Heuer, E. Sarkadi-Nagy, M. Bakacs, S. Tazhibayev, T. Sharmanov, I. Spiroski, M. Beukers, C. van Rossum, M. Ocke, A. K. Lindroos, Eva Warensjö Lemming, J. E. Cade
- Image credit Robina Weermeijer PLOS ONE Functional outcome in home health: Do racial and ethnic minority patients with dementia fare worse? May 26, 2020 Jinjiao Wang, Fang Yu, Xueya Cai, Thomas V. Caprio, Yue Li
- Image credit National Park Service PLOS ONE Barriers & facilitators to healthcare and social services among undocumented Latino(a)/Latinx immigrant clients: Perspectives from frontline service providers in Southeast Michigan June 5, 2020 Monika Doshi, William D. Lopez, Hannah Mesa, Richard Bryce, Ellen Rabinowitz, Raymond Rion, Paul J. Fleming
- Image credit Oriol Portell PLOS ONE ‘One-size doesn’t fit all’: Understanding healthcare practitioners’ perceptions, attitudes and behaviours towards sexual and reproductive health and rights in low resource settings: An exploratory qualitative study June 25, 2020 Gilbert Tumwine, Jack Palmieri, Markus Larsson, Christina Gummesson, Pius Okong, Per-Olof Östergren, Anette Agardh
- Image credit National Cancer Institute PLOS ONE Racial/ethnic disparities in colorectal cancer treatment utilization and phase-specific costs, 2000-2014 April 14, 2020 Angela C. Tramontano, Yufan Chen, Tina R. Watson, Andrew Eckel, Chin Hur, Chung Yin Kong
- Image credit Martha Dominguez de Gouveia PLOS ONE Socioeconomic differences in use of public, occupational and private health care: A register-linkage study of a working-age population in Finland April 16, 2020 Jenni Blomgren, Lauri J. Virta
- Image credit 10.1371/journal.pone.0232462 PLOS ONE The emergence of social gaps in mental health: A longitudinal population study in Sweden, 1900-1959 April 30, 2020 Johan Junkka, Glenn Sandström, Lotta Vikström
- Image credit Ameer Basheer PLOS ONE Defining gentrification for epidemiologic research: A systematic review May 21, 2020 Nrupen A. Bhavsar, Manish Kumar, Laura Richman
- Image credit R O PLOS ONE Socioeconomic disadvantage as a driver of non-urgent emergency department presentations: A retrospective data analysis April 13, 2020 Maria Unwin, Elaine Crisp, Jim Stankovich, Damhnat McCann, Leigh Kinsman
- Image credit Lucas Metz PLOS ONE Higher prevalence of depressed mood in immigrants’ offspring reflects their social conditions in the host country: The HELIUS study June 4, 2020 Karien Stronks, Aydın Şekercan, Marieke Snijder, Anja Lok, Arnoud P. Verhoeff, Anton E. Kunst, Henrike Galenkamp
- Image credit Chris Fuller PLOS ONE Associations between area socioeconomic status, individual mental health, physical activity, diet and change in cardiometabolic risk amongst a cohort of Australian adults: A longitudinal path analysis May 29, 2020 Suzanne J. Carroll, Michael J. Dale, Theophile Niyonsenga, Anne W. Taylor, Mark Daniel
- Image credit Maximillian Conacher PLOS ONE The role of neighbourhood socioeconomic status in large for gestational age June 5, 2020 Farid Boubred, Vanessa Pauly, Fanny Romain, Guillaume Fond, Laurent Boyer
- Image credit Matt Chesin PLOS ONE Neighbourhood property value and type 2 diabetes mellitus in the Maastricht study: A multilevel study June 8, 2020 David Consolazio, Annemarie Koster, Simone Sarti, Miranda T. Schram, Coen D. A. Stehouwer, Erik J. Timmermans, Anke Wesselius, Hans Bosma
- Image credit Jonathan Borba PLOS ONE Relationships between psychosocial stressors among pregnant women in San Francisco: A path analysis June 12, 2020 Stephanie M. Eick, Dana E. Goin, Monika A. Izano, Lara Cushing, Erin DeMicco, Amy M. Padula, Tracey J. Woodruff, Rachel Morello-Frosch
- Image credit Niloy Biswas PLOS ONE Healthcare seeking for chronic illness among adult slum dwellers in Bangladesh: A descriptive cross-sectional study in two urban settings June 15, 2020 Alayne M. Adams, Rubana Islam, Sifat Shahana Yusuf, Anthony Panasci, Nancy Crowell
- Image credit Luis Villasmil PLOS ONE Understanding the role of policy on inequalities in the intergenerational correlation in health and wages: Evidence from the UK from 1991–2017 June 17, 2020 Heather Brown
- Image credit National Cancer Institute PLOS ONE Communication and shared decision-making with patients with limited health literacy; helpful strategies, barriers and suggestions for improvement reported by hospital-based palliative care providers June 19, 2020 Ruud Roodbeen, Astrid Vreke, Gudule Boland, Jany Rademakers, Maria van den Muijsenbergh, Janneke Noordman, Sandra van Dulmen
- Image credit camilo jimenez PLOS ONE Assessing the impact of social determinants of health on predictive models for potentially avoidable 30-day readmission or death June 25, 2020 Yongkang Zhang, Yiye Zhang, Evan Sholle, Sajjad Abedian, Marianne Sharko, Meghan Reading Turchioe, Yiyuan Wu, Jessica S. Ancker
- Image credit Kobby Mendez PLOS ONE Plasma glucocorticogenic activity, race/ethnicity and alcohol intake among San Francisco Bay Area women June 1, 2020 Phum Tachachartvanich, Sylvia S. Sanchez, Scarlett L. Gomez, Esther M. John, Martyn T. Smith, Laura Fejerman
- Image credit Tim Mossholder PLOS ONE Diversity and inclusion for the All of Us research program: A scoping review July 1, 2020 Brandy M. Mapes, Christopher S. Foster, Sheila V. Kusnoor, Marcia I. Epelbaum, Mona AuYoung, Gwynne Jenkins, Maria Lopez-Class, Dara Richardson-Heron, Ahmed Elmi, Karl Surkan, Robert M. Cronin, Consuelo H. Wilkins, Eliseo J. Pérez-Stable, Eric Dishman, Joshua C. Denny, Joni L. Rutter, the All of Us Research Program
- Image credit note thanun PLOS ONE Educational inequalities in mortality amenable to healthcare. A comparison of European healthcare systems July 2, 2020 Håvard T. Rydland, Erlend L. Fjær, Terje A. Eikemo, Tim Huijts, Clare Bambra, Claus Wendt, Ivana Kulhánová, Pekka Martikainen, Chris Dibben, Ramunė Kalėdienė, Carme Borrell, Mall Leinsalu, Matthias Bopp, Johan P. Mackenbach
- Image credit Charu Chaturvedi PLOS ONE Exploring access to government-led support for children with disabilities in Bangladesh July 2, 2020 Reshma Parvin Nuri, Setareh Ghahari, Heather Michelle Aldersey, Ahmed Shafiqul Huque
- Image credit Olga Guryanova PLOS ONE Factors associated with the uptake of cataract surgery and interventions to improve uptake in low- and middle-income countries: A systematic review July 9, 2020 Eunice Wandia Mailu, Bhavisha Virendrakumar, Emma Jolley, Elena Schmidt, Stevens Bechange
- Image credit Ilena George and Daniel Reich, National Institute of Neurological Disorders and Stroke, National Institutes of Health PLOS ONE Health service utilization in immigrants with multiple sclerosis July 9, 2020 Dalia L. Rotstein, Ruth Ann Marrie, Karen Tu, Susan E. Schultz, Kinwah Fung, Colleen J. Maxwell
- Image credit Paweł Czerwiński PLOS ONE Changing social inequalities in smoking, obesity and cause-specific mortality: Cross-national comparisons using compass typology July 10, 2020 Andrea Teng, Tony Blakely, June Atkinson, Ramunė Kalėdienė, Mall Leinsalu, Pekka T. Martikainen, Jitka Rychtaříková, Johan P. Mackenbach
- Image credit Nephron PLOS ONE The role of histology on endometrial cancer survival disparities in diverse Florida July 23, 2020 Ariana L. Johnson, Heidy N. Medina, Matthew P. Schlumbrecht, Isildinha Reis, Erin N. Kobetz, Paulo S. Pinheiro
- Image credit Christina Victoria Craft PLOS ONE Association between over-indebtedness and antidepressant use: A cross-sectional analysis July 24, 2020 Jacqueline Warth, Niklas Beckmann, Marie-Therese Puth, Judith Tillmann, Johannes Porz, Ulrike Zier, Klaus Weckbecker, Birgitta Weltermann, Eva Münster
- Image credit Massimo Sartirana PLOS ONE Associations between social connections, their interactions, and obesity differ by gender: a population-based, cross-sectional analysis of the Canadian Longitudinal Study on Aging July 30, 2020 Zeinab Hosseini, Gerry Veenstra, Nadia Khan, Annalijn Conklin
- Image credit w:User:LinguistAtLarge PLOS ONE Differing interpretations of health care encounters: A qualitative study of non-Latinx health care providers’ perceptions of Latinx patient behaviors August 6, 2020 Lucía Floríndez, Daniella Floríndez, MPH, Dominique Como, MA, OTR/L, Rita Secola, PhD RN CPON FAAN, Leah Duker, PhD OTR/L
- Image credit University of Pennsylvania PLOS ONE Associations between historical redlining and birth outcomes from 2006 through 2015 in California August 7, 2020 Anthony L. Nardone, Joan A. Casey, Kara E. Rudolph, Deborah Karasek, Mahasin Mujahid, Rachel Morello-Frosch
- Image credit Department of Foreign Affairs and Trade PLOS ONE Barriers to accessing maternal health care services in the Chittagong Hill Tracts, Bangladesh: A qualitative descriptive study of Indigenous women’s experiences August 11, 2020 Shahinoor Akter, Kate Davies, Jane Louise Rich, Kerry Jill Inder
- Image credit Elien Dumon PLOS ONE Patterns of multimorbidity and demographic profile of latent classes in a Danish population—A register-based study August 11, 2020 Sanne Pagh Møller, Bjarne Laursen, Caroline Klint Johannesen, Janne S. Tolstrup, Stine Schramm
- Image credit Chronomarchie PLOS ONE Catastrophic health expenditures arising from out-of-pocket payments: Evidence from South African income and expenditure surveys August 11, 2020 Steven F. Koch, Naomi Setshegetso
To keep up to date on the latest research.
PLOS announced the Health Inequities and Disparities Research Call for Papers in October 2019.
PLOS offers a variety of Calls for Papers where selected articles are included in a published Collection. Find out if any of our Calls are relevant to your research.

IMAGES
VIDEO
COMMENTS
Over the past half-century, understanding of health and health care disparities in the United States — including underlying social, clinical, and system-level contributors — has increased.
Work by health inequality researchers is featured in top journals across many fields, including medicine, social epidemiology, political science and sociology, and reducing health inequalities has been put on the agenda in several countries.
HEALTH DISPARITIES, INEQUITY, AND SOCIAL DETERMINANTS: A BRIEF CONTEXT. The urgency to promote health, reduce health disparities, and address the social determinants of health is highlighted in countless reports (Hankivsky and Christoffersen, 2008; World Health Organization, 2006, 2015).
Health inequalities research and health disparities research (hereafter ‘health equity research’) aims to understand, explain and reduce the unequal distribution of health across groups defined by social demographic factors, such as education, income and ethnicity.
This review summarises the present state of research on health inequalities using a social network perspective, and it explores the available studies examining the interrelations of social inequality, social networks, and health.
We found 691 indicators used in the study of health inequalities. The indicators were grouped into 120 topics, 34 of which were selected for having five indicators or more.
In this article, we argue that health inequalities need re-framing to encompass the breadth of disadvantage and difference between healthcare and health outcome inequalities. Second, there needs to be a focus on long-term organisational change to ensure equity is considered in all decisions.
Health disparities persist globally, with certain populations experiencing unequal access to healthcare and poorer health outcomes. This paper provides a comprehensive review of the...
This is the first study to synthesise all published studies and grey literature on the health inequalities strategy conducted in England from 1999 to 2010. This study used a broad search strategy of peer-reviewed and grey literature.
These papers include health equities due to race/ethnicity, socio-economic status, sexual or gender minority identification, immigrant status (including undocumented immigrants), incarceration, socio-economic status, and country of residence.